Toddlers and Button Batteries: A Deadly Combination
Debnath Chatterjee, MD, FAAP, and Alan Jay Schwartz, MD, MSEd
Button battery (BB) ingestions are extremely dangerous and can be life-threatening, especially in toddlers and young children. These BBs are ubiquitous in our homes and are used to power a wide range of electronic devices. Unfortunately, they are easily accessed by young children who like to put these bright shiny objects into their mouths. Previously, Litovitz et al. reported an almost seven-fold increase in deaths and major complications following BB ingestions in children since the introduction of the 20 mm CR 2032 lithium BBs in 2006.1 Further, 12.6% of children <6 years suffered a major complication such as tracheoesophageal fistula, esophageal perforation or stricture, aorto-enteric fistula, and vocal cord paralysis.2
In today’s PAAD, we review a recent publication in Pediatrics and share some good news on legislative efforts to make BBs safer.
Original Publication
Chandler MD, Ilyas K, Jatana KR, et al. Pediatric Battery-Related Emergency Department Visits in the United States: 2010-2019. Pediatrics. 2022;150(3): e2022056709. PMID: 36032018.
Based on data from the National Electronic Injury Surveillance System, there were an estimated 70,322 battery-related emergency department (ED) visits in children < 18 years from 2010-2019, yielding an annual average of 9.5 visits/100,000 children. This roughly translates to 1 battery-related ED visit every 1.25 hours among children < 18 years. The ED visit rate was highest in children < 5 years. Battery ingestions were the most common exposure route, and BB ingestions accounted for 84.5% of the cases. Another scary statistic is that these estimates (2010-2019) were 2.1 times higher compared to the previous study period (1990-2009). Fortunately, there was a decrease in the overall rates of all battery related ED visits from 2017-2019, perhaps signaling a downward trend.
When a BB is lodged in a young child’s esophagus, the mucosa bridges the two terminals allowing current to flow. This leads to the generation of hydroxide radicals (highly alkaline pH), causing liquefactive necrosis and severe tissue injury in as little as 2 hours following ingestion. In both in-vitro and in-vivo studies on piglet esophagus, researchers from the National Button Battery Task Force showed that honey and sucralfate are effective in neutralizing the strong alkali reaction from BB ingestion.3 Based on these studies, the National Capital Poison Center recently updated its BB ingestion guidelines to include the administration of honey at home or en route to the hospital.4 (Link). Two teaspoons or 10 mL of honey may be administered every 10 minutes for a maximum of 6 doses if the child is older than a year of age (since honey can cause botulism in children < 1 year), and a lithium BB has been ingested within the last 12 hours. It is important not to delay taking the child to the closest ED. The administration of honey is not a definitive treatment, and the BB must be removed endoscopically ASAP. At Children’s Hospital Colorado, BB ingestions are treated as trauma-red activations in the ED.
Recent publications in the anesthesia literature summarize the major anesthetic considerations for BB ingestions in children.5-8 The bottom line is DO NOT DELAY the case for NPO status since the risk of ongoing damage to the esophagus far outweighs the risk of pulmonary aspiration. A rapid sequence induction should be performed to facilitate safe endotracheal intubation. Secure additional intravenous access for prolonged ingestions or severe injuries. The maximum amount of damage is seen along the negative pole or narrow end of the battery (Remember the mnemonic: Negative, Narrow, Necrotic). During BB removal, if the negative pole faces anteriorly, a rigid bronchoscopy should also be performed to rule out tracheal injury.
A team from Children’s Hospital Colorado recently created a couple of infographics- one for parents and another one for anesthesia providers to highlight the dangers of BB ingestion in young children. These infographics are posted on the SPA website and published in a recent APSF newsletter.9 Please feel free to share these infographics and educate your friends, colleagues, and local media outlets.
Now for the good news! Reese’s Law is a bill that requires the Consumer Product Safety Commission to establish safety standards for BBs. Specifically, products with BB must include a warning label instructing consumers to keep the BB out of reach of children and a battery compartment that prevents access to the BB by children < 6 years. Named in honor of Reese Hamsmith, an 18-month-old girl from Texas who died following a BB ingestion, this bipartisan bill recently passed through the House and Senate and is one step closer to becoming a law. Link. We desperately need stronger regulations and safety standards for BBs.
References
1. Litovitz T, Whitaker N, Clark L, et al. Emerging Battery-Ingestion Hazard: Clinical Implications. Pediatrics. 2010; 125:1168-77. PubMed
2. Chandler MD, Ilyas K, Jatana KR, et al. Pediatric Battery-Related Emergency Department Visits in the United States: 2010-2019. Pediatrics. 2022;150(3): e2022056709. PubMed
3. Anfang RR, Jatana KR, Linn RL, Rhoades K, Fry J, Jacobs IN. pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury. Laryngoscope 2019; 129(1): 49-57. PubMed
4. National Capital Poison Center Button Battery Ingestion Triage and Treatment Guideline. www.poison.org/battery/guideline. Accessed Sept 7th, 2022.
5. Hoagland MA, Ing RJ, Jatana KR, Jacobs IN, Chatterjee D. Anesthetic Implications of the New Guidelines for Button Battery Ingestion in Children. Anesth Analg. 2020;130(3): 665-72. PubMed
6. Eck JB, Warwick AA. Anesthetic Implications of Button Battery Ingestion in Children. Anesthesiology. 2020; 132(4):917-24. PubMed
7. Pae SJ, Habte SH, McCloskey JJ, Schwartz AJ. Battery Ingestion Resulting in an Aortoesophageal Fistula. Anesthesiology. 2012; 117: 1354. PubMed
8. Templeton TW, Terry BJ, Pecorlla SH, Downard MG. Button Battery Ingestion, A Ture Surgical and Anesthetic Emergency. Anesthesiology. 2020; 132: 581.PubMed
9. Hoagland MA, Ing RJ, Chatterjee D. Perioperative Management of Button Battery Ingestions in Children. APSF Newsletter. February 2022. Link
Conflict of Interest: DC represents the AAP Section on Anesthesiology at the National Button Battery Task Force. AJS attests to no conflict of interest.
PS from Myron
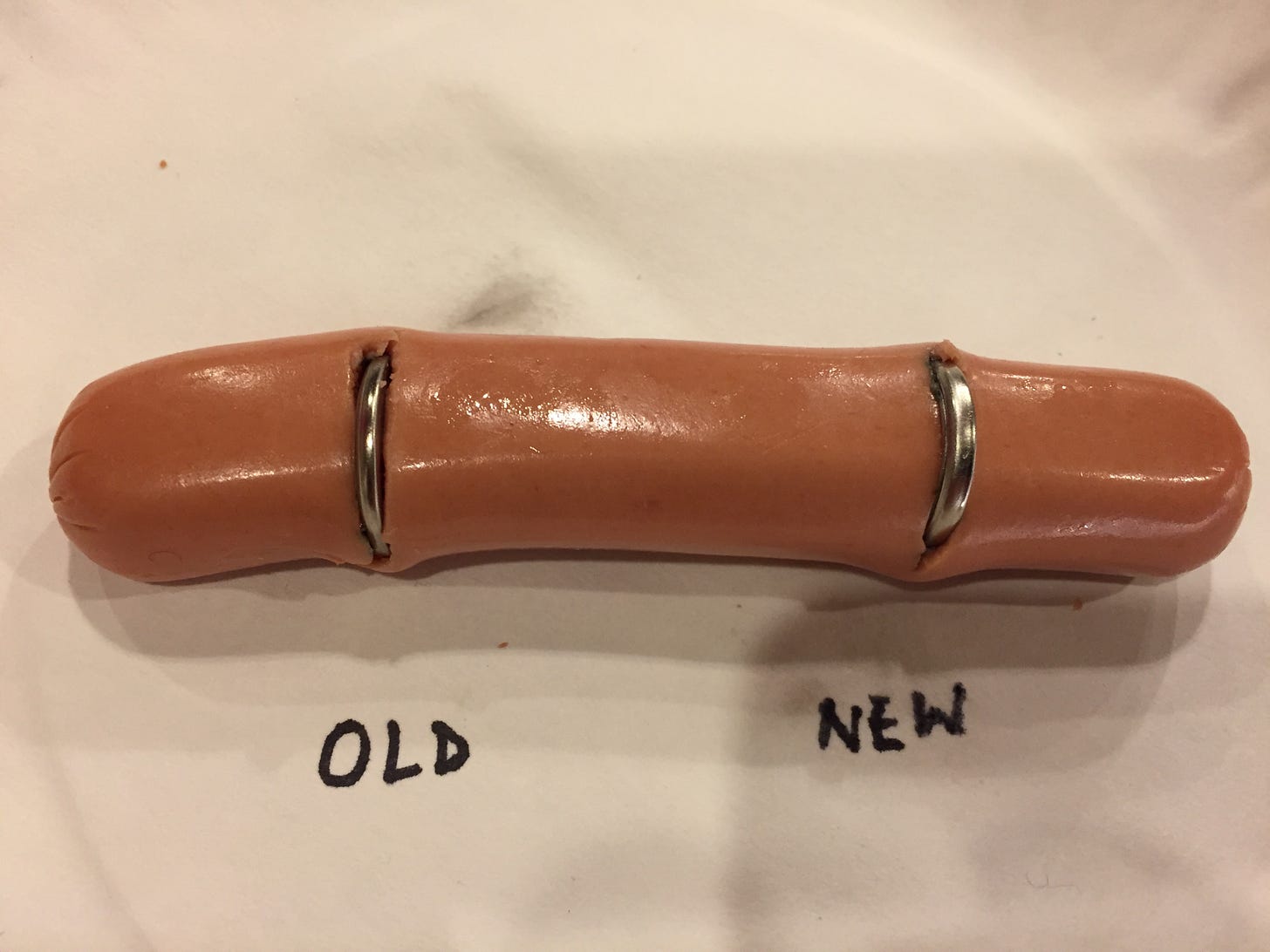
When I first heard about the dangers from button battery ingestion about 5 years ago, I thought “can it really be that bad”? Then I saw these pictures from Dabe Chatterjee’s son’s 5th grade science project in which Dabe’s son Rohan inserted new and old button batteries into hot dogs and with time lapsed photography looked at what if any damage would occur. Well, if you didn’t think these batteries could cause enormous damage these pictures are worth a thousand words! Rohan is now a junior in high school.
TIME ZERO
TIME 90 MINUTES