Respiratory adverse events after LMA removal: Does the anesthetic make a difference? YES!!
John E. Fiadjoe MD
Original article
Karam C, Zeeni C, Yazbeck-Karam V, Shebbo FM, Khalili A, Abi Raad SG, Beresian J, Aouad MT, Kaddoum R. Respiratory Adverse Events After LMA® Mask Removal in Children: A Randomized Trial Comparing Propofol to Sevoflurane. Anesth Analg. 2023 Jan 1;136(1):25-33. doi: 10.1213/ANE.0000000000005945. Epub 2022 Feb 25. PMID: 35213484.
I used to be skeptical about the benefits of TIVA in pediatric anesthesia. I remember Dr. Mark Ansermino from British Columbia’s Children’s Hospital sharing data at a SPA meeting about the benefits seen in their practice as it evolved to doing more TIVA. I decided after that meeting to try using TIVA for the next few weeks. I quickly earned the reputation of being the anesthesiologist whose patients moved during surgery – a Fiadjoe Anesthetic was all that needed to be said. I did have an interesting interaction during those weeks that I’ve never forgotten. After one of those propofol based anesthetics, I got the dreaded call from the PACU “Your last patients mom wants to speak to you”. My negativity bias kicked in and I rushed over expecting some postop concern - “my kid could solve differential equations before your anesthetic but can barely do Calculus now”! What I got was “My kid has had 7 anesthetics here and has never woken up this smoothly, you did something different! What did you do?” I responded “ Oh I just used a slightly different anesthetic” she responded ”Great! I’m requesting you for all his future surgeries”. There was born my TIVA cohort of patients.
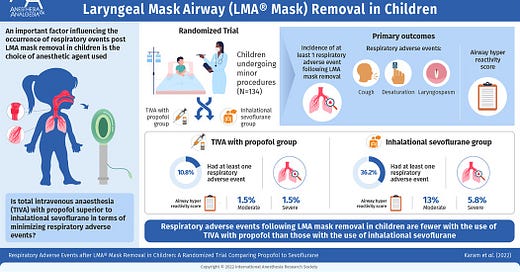
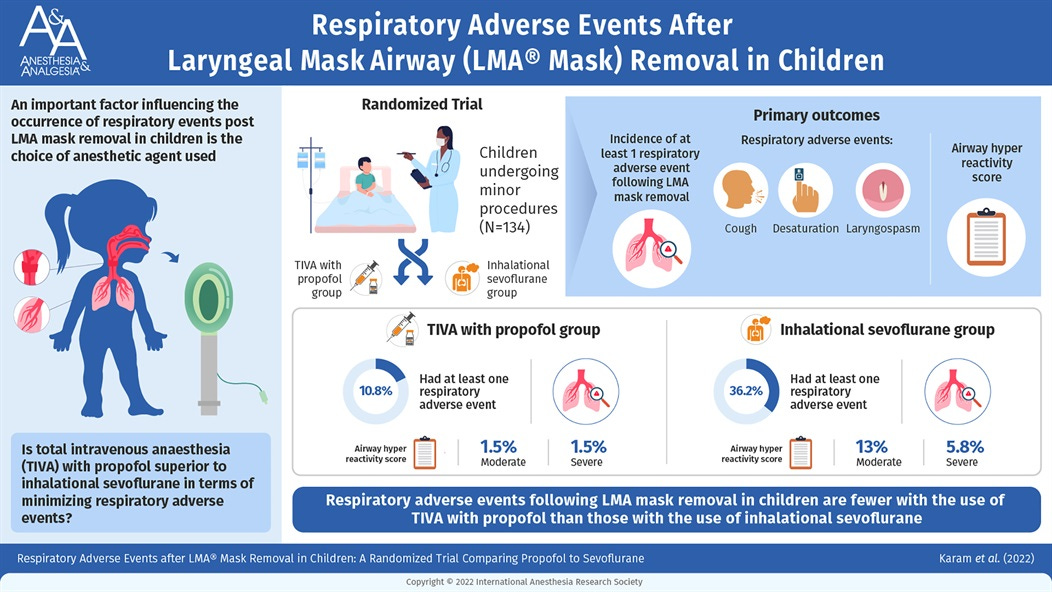
Today’s PAAD is an interesting prospective, randomized, double-blind clinical trial comparing respiratory adverse events after LMA removal in children 6 months to 7 years old who received general anesthesia using TIVA with Propofol vs Sevoflurane. What was unique about this study was that the respiratory adverse events were assessed by a blinded clinician who had no idea which anesthetic technique was used. The definition of respiratory adverse events varies across studies and sometimes outcomes included in many studies are more nuisances than harmful. The outcomes chosen in this study included LMA mask biting or teeth clenching -nuisance-ish i.e. unless you don’t fix it, breath holding (>5secs) – nuisance-ish, Laryngospasm- problem!, bronchospasm – problem!, desaturation spo2 <95% - problem-ish and upper airway obstruction- nuisance, cough – nuisance.
The study randomized 134 patients to the Sevoflurane vs Propofol groups and found that children in the propofol group had significantly lower incidence of respiratory adverse events 10.8% vs 36.2%; relative risk 0.29;95% CI (0.14-0.64); P=0.001. There was less coughing, laryngospasm, and desaturation in the Propofol group. The Sevo group had 7 cases of laryngospasm vs 1 in the propofol group. Although the laryngospasm incidence in the Sevoflurane group seems high to me, anecdotally, I have encountered less laryngospasm when I use a TIVA based anesthetic. These days I use EEG and neuromuscular blocking drugs to keep the surgeons happy. Other purported benefits of TIVA include less emergence agitation (seen in this study as well), less PONV, less immune suppression? (novel work from Dr. Koichi Yuki’s lab) less impairment of ciliary motility, less environmental impact?, more alert patients after recovery? And on and on…
What is your experience with TIVA? benefit, mostly hogwash or something in between? Send your responses to Myron who will post in a Friday reader response.