Remembering the classics: T wave changes to detect intravascular injections of local anesthetics with epinephrine
Quentin A. Fisher
In a recent PAAD, “Alpha-1-acid glycoprotein and local anesthetics in the neonate”, June 22, 2023, I mentioned the discovery by Dr. Quentin Fisher that intravascular injection of local anesthetics with epinephrine would produce changes in T waves on the ECG and monitoring the ECG during fractionated, divided doses could reduce the risk of toxicity. As I wrote that introduction, I realized that many of you may not know this study nor its origins, so I asked Dr. Fisher to revisit this classic paper for the PAAD readership and to give us his insights in how and why he did the study. Myron Yaster MD
Original article
Fisher QA, Shaffner DH, Yaster M. Detection of intravascular injection of regional anaesthetics in children. Can J Anaesth. 1997 Jun;44(6):592-8. PMID: 9187777
I was managing a patient in whom I seemingly fell behind in tracking fluid deficits, and decided to give a temporizing pressor. Conventional wisdom taught that epi was “Nature’s own” presssor of choice, ephedirne being more unpredictable in children. After the epi dose, blood pressure improved but I noticed - with some angst - tall peaked T-waves on the ECG, which resolved quickly. The case proceeded uneventfully. The next occasion I had to use epi, I noticed the same phenomenon. On checking with the adult electrophysiologists, they directed me to a wealth of literature showing T-wave flattening with epinephrine, which was commonly used as an infusion (not a bolus) to test antiarrhythmics.
There was no immediate explanation for the T-wave changes, but it occurred to me that this might be useful in monitoring test doses for caudal injections. Previously, most Peds anesthesiologists seemed to monitor only for blood aspiration, or heart rate change (blood pressure changes being too evanescent to capture); pretreatment with atropine was common (but of note, some of my fellowship mentors did not use epinephrine, depending on blood aspiration and the ”feel” of injection).
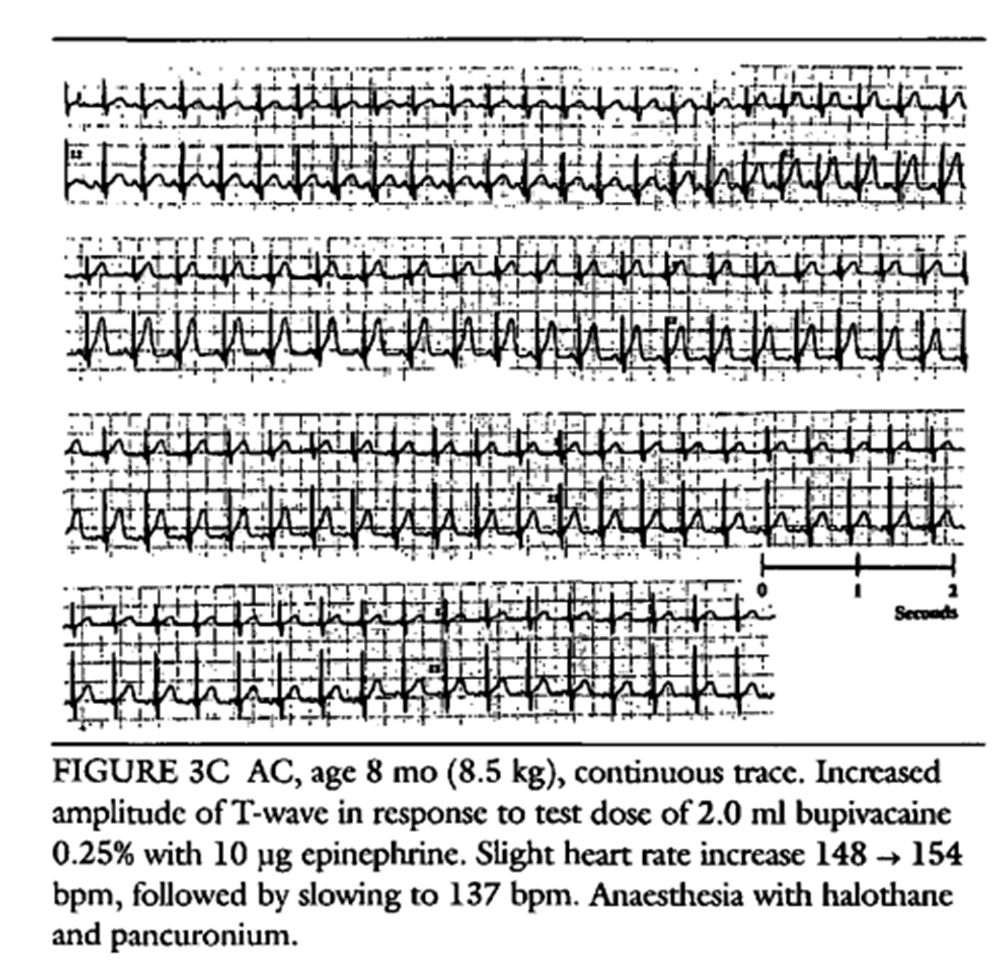
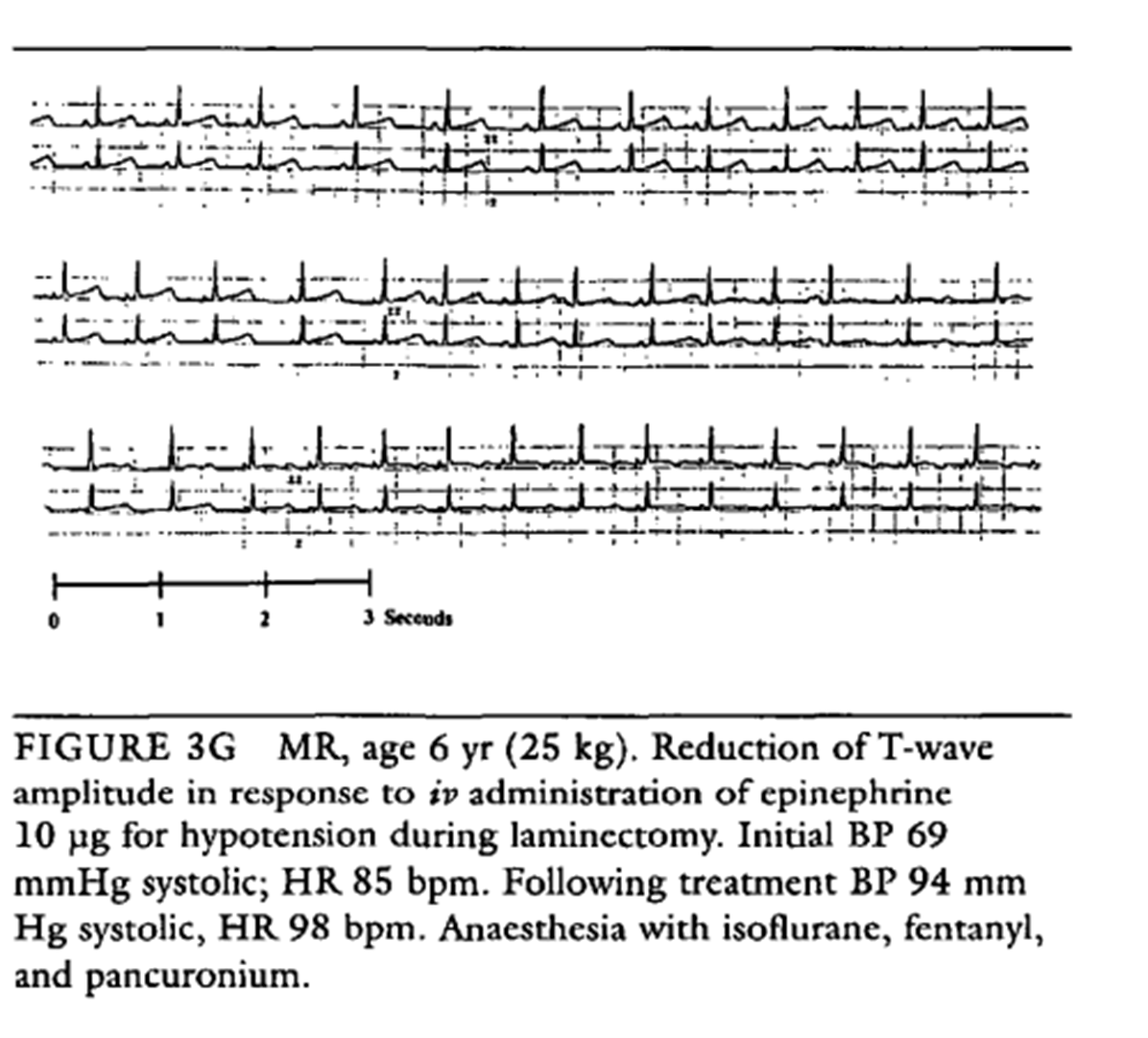
After some informal observations during caudal injections, we organized a simple observational study to print ECG strips on every pediatric patient having an epidural injection of bupivacaine with epinephrine. The resident marked each strip with relevant clinical information. A total of 742 injections by needle or catheter were tracked. Intravascular injection was diagnosed by blood aspiration (not all had diagnostic HR changes) or HR in 5.6% of cases. All showed T-wave peaking or inversion. (see figures below from the paper) Intravascular injection seemed more likely in catheter placements than single shot needle (7.6% vrs 3.8%), though the numbers were too small to assert a statistical difference. Interestingly, we informally noticed that most blood aspirations were evident only after the test dose was completed. We found that reliance on blood aspiration alone would have missed over 50% of proven intravascular injection, and reliance on HR would have missed 17%.
We concluded that epinephrine should be used as a marker in test-dosing; dosing should be fractionated; aspiration for blood should be done both before and after the test and before subsequent fractions; and monitoring the ECG is a useful addition to track inadvertent intravascular injection.
We were not the first to notice this phenomenon. Fried et al (Anesthesiol 1993;79:394) reported it in an anecdotal report of five cases but suspected it was an indicator of a bupivacaine cardiac effect. Our study conclusively showed it was the epi.
Our findings also provided a route to resolve ambiguous test dose results. When the heart rate does not achieve a threshhold of >10bpm, or ECG findings only look suspicious, a second test dose using a somewhat larger dose of only epinephrine often helps resolve the ambiguity without the risk of LA toxicity.
Many questions remained unanswered. If only part of the test dose actually enters the bloodstream, what is the minimal effective dose of epinephrine to detect intravascular injection? In our practice we could not ethically give measured IV doses of bupivacaine with epinephrine to children, but several studies by Tanaka et al. confirmed the effects of epinephrine on T waves.1-3 Why does epinephrine flatten the T-wave with infusions but cause peaking with bolus? Is there tachyphylaxis after more than one epi test? Is the test reliability different with vapor or TIVA-based anesthetics? And finally, how long had this been going on and why did we never notice it?!
I learned a few things from this exercise. First, simple clinical observations can lead to new avenues of inquiry. Second, it is possible to do a reasonable clinical study with the patients we see every day. This type of study that wrapped into our daily work, required no grant (which, by the way, was something of a disadvantage when it came time for promotion review), and cost little in effort or clinical time for the cases that were recorded.
References
1. Tanaka M, Nishikawa T. Evaluating T-wave amplitude as a guide for detecting intravascular injection of a test dose in anesthetized children. AnesthAnalg. 4/1999 1999;88(4):754-758. Not in File.
2. Tanaka M, Goyagi T, Kimura T, Nishikawa T. The efficacy of hemodynamic and T wave criteria for detecting intravascular injection of epinephrine test doses in anesthetized adults: a dose-response study. AnesthAnalg. 11/2000 2000;91(5):1196-1202. Not in File.
3. Tanaka M, Kimura T, Goyagi T, Ogasawara K, Nitta R, Nishikawa T. Evaluating hemodynamic and T wave criteria of simulated intravascular test doses using bupivacaine or isoproterenol in anesthetized children. AnesthAnalg. 9/2000 2000;91(3):567-572. Not in File.