Remembering the classics : Citrate Toxicity and Fresh Frozen Plasma and other Badness!
Charles Coté MD
As discussed in a PAAD last month, I recently had the opportunity of reading and reviewing the 3d edition of (Ron) Litman’s Basics of Pediatric Anesthesia for the journal Anesthesiology. I’ll have more to say about that when the review is accepted and published by the journal. Admittedly this was the first time I read a textbook from cover to cover since I studied for my own written Boards several decades ago. It afforded me the opportunity to rediscover classic articles that we haven’t covered in previous PAADs. One topic I was particularly looking for was the management of pediatric burn patients. There are several recurrent themes in the perioperative management of pediatric burns including: how to assess the extent of the burn, how to monitor when there isn’t a hell of a lot of real estate to attach monitors, blood and fluid management, hypermetabolism, drugs to use and not use for neuromuscular blockade, temperature and pain management to name just a few. In looking through the book chapter’s reference list, I found several “classic” articles and not surprisingly, some by a frequent PAAD contributor Dr, Charles (Charlie) Coté.1 I asked him to look thru his CV to find one or two of his most important papers as “a remembering the classics” for the PAAD readership. Last month he discussed platelets and blood loss. Today he will review his original article on Citrate Toxicity and Fresh Frozen Plasma.2 Myron Yaster MD
Original article
Coté CJ, Drop LJ, Hoaglin DC, Daniels AL, Young ET. Ionized hypocalcemia after fresh frozen plasma administration to thermally injured children: effects of infusion rate, duration, and treatment with calcium chloride. Anesth Analg. 1988 Feb;67(2):152-60. PMID: 3277480.
In 1979 I was assigned to the Shriners Burns Institute, and I had had no prior experience caring for children with burns. This was pre-HIV so the surgeons had a reputation of losing a lot of blood, 1-3 blood volumes per trip to the OR for major burns. We started a case of an ~8kg infant and I went to start a second room when I was stat paged back to room 1 where I found the infant in electromechanical dissociation and ongoing chest compressions; the surgeon had not yet started. In asking my resident what transpired he informed me that he had given a unit of FFP under pressure over several minutes anticipating massive blood loss and wanting to assure an adequate blood volume. The cause was obvious, a sudden citrate load from the FFP inducing severe ionized hypocalcemia which rapidly responded to several doses of calcium and no harm done.
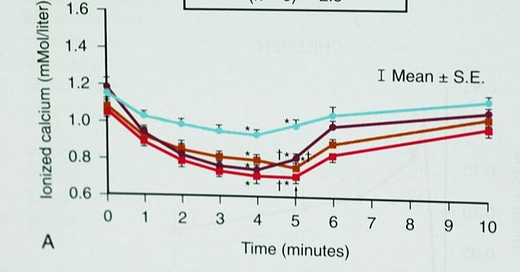
This event triggered my interest, and after IRB approval and informed consents, we began a measured study whereby the IRB allowed me to study 6 children then report back before further studies. All children were fully monitored with arterial and central lines. We used a large 4-barrel Harvard pump with a series of 4 way stop cocks and extension tubings to allow us to administer the FFP in large quantities and at a steady rate. I first studied 6 children administering 1 mL/kg/minute for 5 minutes then stopping the infusion. The IRB the approved study of 3 additional rates: 1.5, 2.0, 2.5 mL/kg/minute. As expected, we found profound reductions in ionized calcium but unexpectedly there were no adverse cardiovascular responses. More on this later. Of particular note was that the ionized calcium values rapidly returned to baseline within 5 minutes of stopping the FFP with no exogenous calcium administered (Figure 1).
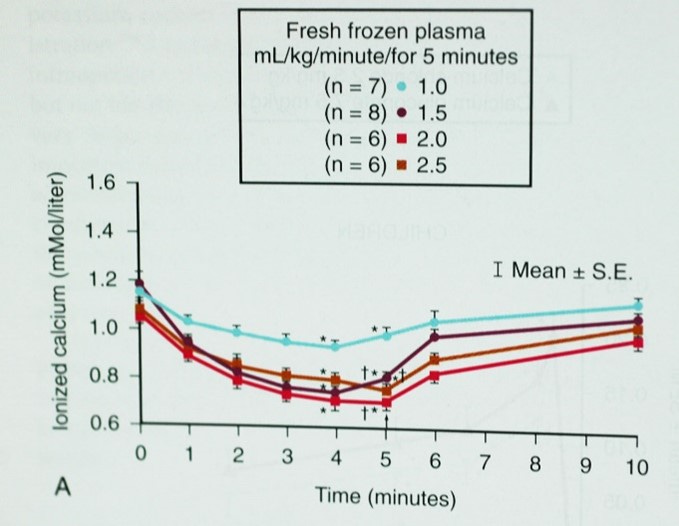
We also studied several children where we administered exogenous calcium at 2 minutes into the FFP infusion and this blunted the more severe reductions we had previously observed (Figure 2).2
Several important conclusions followed: 1) rapid and profound reductions ionized calcium occur even with rates as slow as 1mL/kg/minute (now imagine trying to give this slow rate to a 2 kg neonate, very difficult and the reason that neonates and toddlers are so vulnerable to these adverse responses when administering FFP. 2) the rapid return of ionized calcium after stopping the infusions likely related to the very rapid metabolism of citrate in the liver. 3) this rapid metabolism was most likely related to the hypermetabolic state of burned children; this rapid return to baseline values would not be so profound in children with normal metabolic rates and thus they are at greater risk than the children with burns.
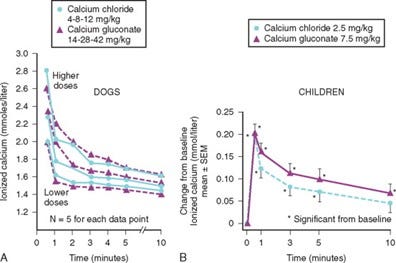
We then conducted a study to determine if there was any difference in administering calcium chloride or calcium gluconate in terms of rapid rise of ionized calcium.3 As a pediatrician I had been taught to always use gluconate as it was less sclerosing to tissue and as an anesthesia resident I was taught to always administer calcium chloride because it does not need liver metabolism to free up the ionized calcium and therefore it would have a more rapid onset. Well, both of those teachings were incorrect. The literature has as many case reports about sloughed tissue with both formulations. So, we studied it in both a dog model and in the children with burns. We found that if equi-ionizable doses of each formulation was administered, then there was no difference in ionized calcium at 30 seconds after administration (Figure 3).
Thus, we totally disproved that hepatic metabolism was needed with calcium gluconate and that either formulation would be effective as long as equi-ionized doses were administered (e.g., 5 mg/kg calcium chloride = 15 mg/kg calcium gluconate). So whichever formulation one has at hand will be equally effective.
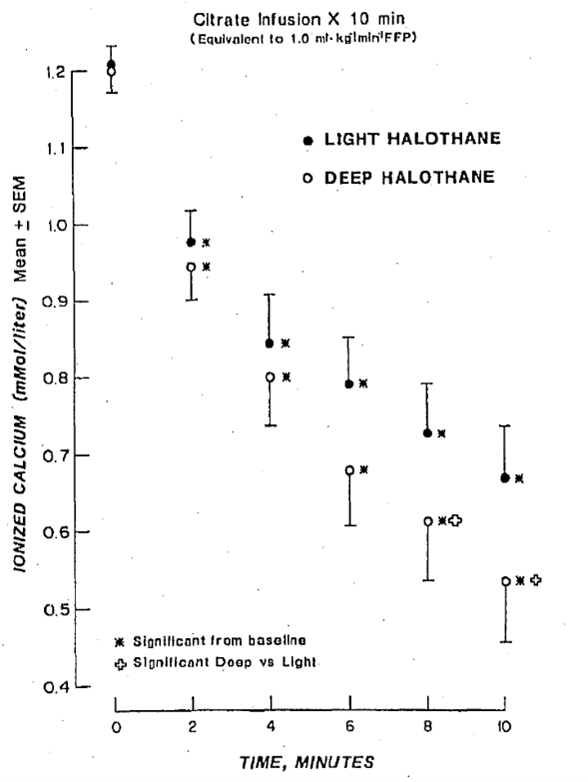
We then conducted another study in a dog model examining the cardiovascular responses to citrate infusions with a deep plane of halothane and a light plane of halothane anesthesia. All dogs demonstrated profound adverse cardiovascular responses which were greater during deep halothane (all dogs suffered cardiac arrest before the end of the planned 20-minute citrate infusions); those that were deeply anesthetized also experienced more profound reductions in ionized calcium.4 The take home message is 1) ionized hypocalcemia occurs pari passu with citrate dose 2) more profound adverse cardiovascular responses (hypotension decreased cardiac output) secondary to a greater fall ionized calcium will occur during deeper planes of halothane anesthesia (Figure 4).
Since all inhalation agents are calcium channel blockers (even sevoflurane or desflurane) ionized hypocalcemia potentiates the myocardial depression of calcium blockade from inhalation agents 3) the greater fall in ionized calcium during deeper planes of halothane anesthesia may reflect shunting of blood away from splanchnic organs (liver) resulting in decreased metabolism 4) mixing inhalation agent with a sudden citrate load is a bad combination and a disaster waiting to happen (Figure 5).
The bottom line if you anticipate a procedure to involve significant and/or possible rapid blood loss, minimize the dose of inhalation agent or avoid entirely. This is especially important in neonates and toddlers where is quite easy to administer FFP at rates > 1 mL:/kg/min. If your patient experiences an adverse response give calcium, calcium, calcium (with chest compressions) until there is return of circulation!
Send your thoughts and comments to Myron who will publish in a Friday reader response.
References
1. Firth PG, Mai CL. The evolution of pediatric sedation and anesthesia patient safety: An interview with Dr Charles J. "Charlie" Coté. Paediatric anaesthesia 2020;30(11):1183-1190. (In eng). DOI: 10.1111/pan.13999.
2. Cote CJ, Drop LJ, Hoaglin DC, Daniels AL, Young ET. Ionized hypocalcemia after fresh frozen plasma administration to thermally injured children: effects of infusion rate, duration, and treatment with calcium chloride. AnesthAnalg 1988;67(2):152-160.
3. Cote' CJ, Drop LJ, Daniels AL, Hoaglin DC. Calcium chloride versus calcium gluconate: comparison of ionization and cardiovascular effects in children and dogs. Anesthesiology 1987;66(4):465-470.
4. Cote' CJ. Depth of halothane anesthesia potentiates citrate-induced ionized hypocalcemia and adverse cardiovascular events in dogs. Anesthesiology 1987;67(5):676-680.