From Carole Lin MD Clinical Associate Professor of Anesthesiology, Stanford University on the June 11 PAAD: Suprazygomatic Maxillary Nerve Blocks for pediatric T&A. Carole was the first author of the reviewed paper.
When considering any procedure, we must consider if the proverbial juice is worth the squeeze. In our study, we found that patients who received a nerve block, on average, used less than half the opiates of the control group. Additionally, more than half of the patients in the block group required no opiates in PACU compared to 26% in the control group. Perhaps most importantly, patients who received a nerve block had FLACC scores less than half of those in the control group. Although unreported in our publication, we saw 4 patients in the control group readmitted, while none in the block group required readmission. We theorize this may be due to improved hydration and better-controlled pain on the first postoperative day.
These benefits must be weighed against the risks of performing the nerve block and the time it takes to do the block. Our study found no additional complications from performing the nerve block. In response to the concern about the 17-minute block time during fast-paced adenotonsillectomy cases, we acknowledge the study's findings that patients in the block group spent an average of 82.4 minutes in the operating room compared to 65.5 minutes in the control group (mean difference 16.8, 95% CI, 6.3 to 27.3; Cohen d, -0.32). It is important to note that this study was not designed to evaluate block performance time, and the overall OR time was used as a proxy. The additional time can be attributed to several factors, including educational efforts, procedural timeouts, and the coordination of teams before and after the procedure. As an example, our study was performed at an academic medical center, and blocks were demonstrated to resident physicians. Even so, the effect size of this extra time was small (Cohen’s d 0.3).
It is important to note that the ultrasound-guided approach can be performed efficiently when requiring equipment readiness. Practitioners familiar with this block, such as those routinely performing cleft palate/lip repair, can complete the procedure more quickly. Experience supports that bilateral blocks done by landmark without ultrasound can be completed form this block efficiently without significantly disrupting workflow.
Further studies are needed to identify which patients would benefit most from this peripheral nerve block. This research should include a more detailed analysis of OSA severity and other comorbidities where narcotic avoidance is particularly beneficial in reducing
Follow up on PAAD Does timing of inguinal hernia repair in preterm infants influence serious adverse effects? April 17, 2024
Does timing of inguinal hernia repair in preterm infants influence serious adverse effects?
Inguinal hernia repair is one of the most common surgeries performed in preterm infants. Whether the inguinal hernia should be repaired prior to or after discharge from the neonatal intensive care unit is controversial: either alternative can result in adverse events.
Dr Bishr Haydar found the following response to the original article:
Montalva L, Clariot S, Bonnard A. Early vs Late Inguinal Hernia Repair in Preterm Infants. JAMA. 2024 Jun 17. doi: 10.1001/jama.2024.10099. Epub ahead of print. PMID: 38884959.
As I (MY) hope you recall the original article by HIP Trial Investigators; Blakely ML et al: Effect of Early vs Late Inguinal Hernia Repair on Serious Adverse Event Rates in Preterm Infants: A Randomized Clinical Trial. JAMA. 2024 Mar 26;331(12):1035-1044. doi: 10.1001/jama.2024.2302. PMID: 38530261; PMCID: PMC10966421 found that early surgical repair of neonatal inguinal hernias was associated with more complications than later repair and recommended later repair. There were a lot of problems with that study (see the original PAAD, link above). Montalay et al reveal that 99% of the infants in the study underwent their repairs under general anesthesia and that preterm infants undergoing general anesthesia are prone to postoperative apnea and bradycardia. They, like we, wonder if the results would be the same if these infants underwent their repairs under spinal anesthesia.
From Kirk Lalwani, MD, FRCA, MCR, FASA, Professor of Anesthesiology and Pediatrics, Director, Pediatric Anesthesiology Fellowship Program, Anesthesiology and Perioperative Medicine, Oregon Health and Science University, Portland, OR 97239 on setting up a Roth IRA for your kids
Just wanted to point out that the IRS only allows Roth funding amounts that are equivalent to what your teenager has earned in the tax year, and no more. So, if your kid earns $4000 all year from his or her summer job, that's the maximum that can be contributed to a Roth IRA for that year (no matter who funds it).
Second, as of 2024, leftover 529 College Saving plan contributions that have been in a 529 plan account that has existed in the same beneficiary's name for at least 15 years, and the money in the account for at least 5 years, can be rolled over to fund a Roth IRA up to the maximum earned by the individual, subject to some conditions, as detailed in the link below. This is a great option to help them fund their Roth's with leftover 529 plan funds which would otherwise be subject to penalties and taxes if withdrawn for non-educational purposes.
https://www.fidelity.com/learning-center/personal-finance/529-rollover-to-roth
From Travis Lee Reece-Nguyen MD, MPH, FAAP Stanford University, Chair Diversity, Equity, and Inclusion Committee, Society for Pediatric Anesthesia and Annery Garcia-Marcinkiewicz MD Children’s Hospital of Philadelphia
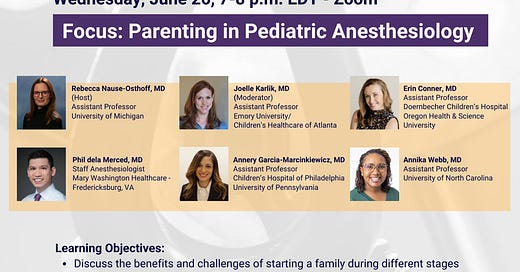
Have you ever wondered about starting a family while in your Pediatric Anesthesia career journey? What are some things you’d like to know from colleagues on this rewarding yet challenging journey? Register with the QR code below to hear some perspectives and join in on the conversation. Spoiler alert (from AGM)- there is no such thing as the “right” time!
SPAERS is hosting a SPA Spotlight webinar series called Parenting in Pediatric Anesthesiology. Our panel of pediatric anesthesiologists from around the country will discuss their paths in the field and their parenting stories, challenges, and successes. The panel is focused on medical students and residents interested in pediatric anesthesiology!
u