Radiation safety
Myron Yaster MD, Eddy Zandee van Rilland MD, and Genie Heitmiller MD
In a survey study performed several years ago, my co-authors and I (MY) found that “few pediatric anesthesiologists had ever received formal training in radiation safety and few routinely adhered to preventative strategies to minimize the risk of radiation-induced injury, particularly the routine use of dosimeters, lead glasses, and thyroid and lead acrylic shields.”[1] Six years later, the need to improve radiation safety education, to change the safety culture surrounding radiation safety, and to more fully investigate the utility of dosimeters and barriers to routine use of lead shielding and leaded eye protection in pediatric anesthesia practice remain the same as it was then.
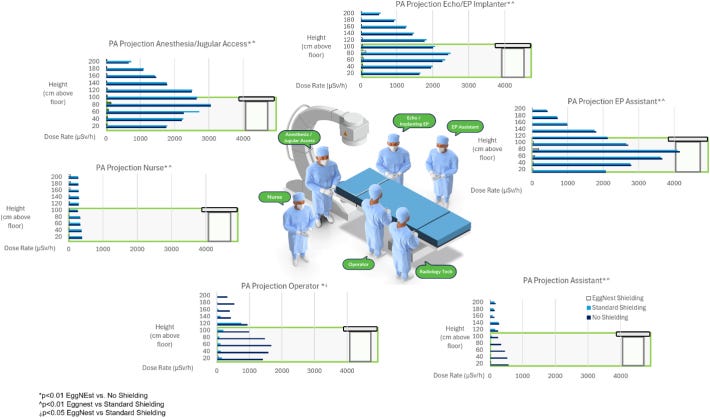
In today’s PAAD, Riley et al.[2] compared the effectiveness of two new radiation shielding systems in protecting ALL of the health care workers from ionizing radiation in interventional cardiology suites. As a review, during radiologic procedures, personnel may be exposed to three different types of ionizing radiation: the primary x-ray beam, scattered x-rays, and leakage from the x-ray equipment itself. Unlike surgeons or interventional radiologists and cardiologists whose hands or bodies may be directly exposed to x-rays in the performance of procedures, pediatric anesthesiologists are rarely directly exposed to the primary x-ray beam. And leakage from properly maintained equipment should be minimal. As today’s PAAD shows, anesthesiologists (and interventionalists working at the head of the bed while performing jugular vein cannulation) have the highest exposure to scatter radiation (Figure below). What, you may ask, is “scatter radiation”? Scatter radiation occurs when the x-ray beam interacts with body tissues and disperses in different directions. This phenomenon contributes significantly to occupational exposure for healthcare staff. Thus, scatter from the patient and the operating/imaging table is the most important source of radiation exposure and can be limited by distance, duration of exposure, shielding, and training.[1]
Why should you care? “Scatter radiation exposure for personnel in the procedure room has been associated with a 3-fold increase in the incidence of various cancers and a 6-fold increase in the incidence of cataracts.”[2, 3] And of course many pediatric anesthesiologists are women and radiation exposure during pregnancy is obviously of great concern. In today’s PAAD, we will focus on passive and active methods of radiation protection. But for those of you wanting to take a deeper dive or want to discuss many of these issues more formally in a journal club setting or while teaching trainees in the OR, a really good resource and starting point is the article by Whitney et al. Myron Yaster MD
Original article
Riley RF, Kamen J, Tao A, Gomez-Cardona D. Comparative effectiveness of the EggNest complete shielding system to standard shielding in the Cath lab. Am Heart J Plus. 2025 Apr 10;54:100543. doi: 10.1016/j.ahjo.2025.100543. PMID: 40276545; PMCID: PMC12017850.
In safety engineering you can use passive and active measures. Think childproofing your home. Passive childproofing aims to prevent hazards from occurring. Examples include installing safety gates at the top and bottom of stairs to prevent falls. Active childproofing focuses on stopping a hazard from causing injury if encountered. Examples include supervising children directly when they are near water (e.g., bathtub, swimming pool). Similarly, in engineering radiation safety for health care workers, passive radiation safety measures include shielding the environment (lead-lined walls and doors), built-in features in x-ray equipment that reduce patient and health care worker exposure, like timers and automatic exposure control, and dosimeters that record cumulative radiation exposure. Active radiation safety measures include wearing wrap around lead aprons, thyroid shields and leaded eyewear and keeping exposure as low as reasonably achievable (ALARA) via minimizing the duration of exposure, maximizing the distance from the ionizing source, and shielding (mobile barriers, table shields, tube shielding that is built into the x-ray tube, and personal protective equipment.) Finally, a crucial piece in active measures is proper training and education, which as Whitney et al. found, is sorely lacking. Indeed, today’s PAAD may be a good incentive to review your own training and education!
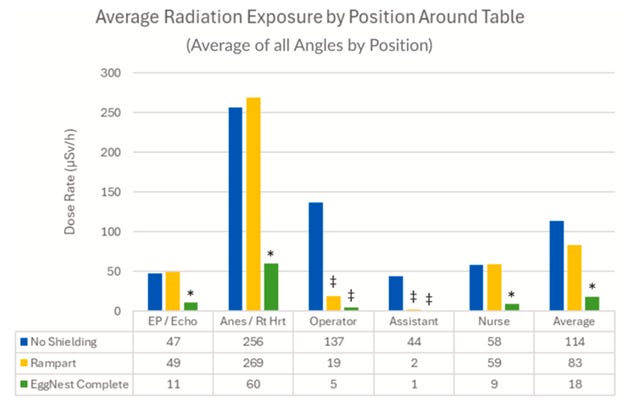
In today’s PAAD, Riley et al investigated the amount of scatter radiation comparing no shielding with two shielding systems: the Rampart IC system and the EggNest Complete system. What did they find? First, they found that the anesthesiologist position had the highest amount of scatter radiation exposure when compared to other positions around the table and the room – almost twice as much as the operator and five times as the rest of the room. Next they found that when measuring the scatter radiation for the anesthesiologist’s position with the EggNest Complete Shielding “there were substantial reductions in scatter radiation measurements compared to no shielding and the Rampart IC system for these positions (average of all 3 positions in all angulations: 27 ±56 using the EggNest Complete vs 131 ±157 μSv/h using the Rampart IC system, an 80% overall reduction when testing the EggNest Complete compared to no shielding and Rampart IC, P <.01). It should be noted that this study was funded by EggNest and one of the authors serves as an advisor for the company. Nevertheless, the important point is that the anesthesiologist has significantly more exposure to scatter radiation than anyone else in the room.
We suspect that it is very unlikely that you have the Eggnest complete shielding system in your catheterization and interventional radiology suites. We are highlighting the article to underscore the need for wearing protective shielding AND mobile barriers in your practice because of the high amount of radiation scatter at the head of the bed….the position in which we are located.
If you are interested in learning more about radiation safety, you might want to take a peek at a recent article on Principles of Radiation Safety for Anaesthetists published this year in BJA Education [4].
Do you have ongoing or really any training in radiation safety in your practice? Are you being supplied with dosimeters? Do you have easy access to, or your own, personal wrap around lead? Do you wear leaded protective eyewear? If you are a pregnant woman do you ask or can you opt out of radiology suite cases? Send your thoughts and comments to Myron (myasterster@gmail.com) who will post in a Friday reader response.
References
1. Whitney GM, Thomas JJ, Austin TM, Fanfan J, Yaster M: Radiation Safety Perceptions and Practices Among Pediatric Anesthesiologists: A Survey of the Physician Membership of the Society for Pediatric Anesthesia. Anesthesia and analgesia 2019, 128(6):1242–1248.
2. Riley RF, Kamen J, Tao A, Gomez-Cardona D: Comparative effectiveness of the EggNest complete shielding system to standard shielding in the Cath lab. Am Heart J Plus 2025, 54:100543.
3. Andreassi MG, Piccaluga E, Guagliumi G, Del Greco M, Gaita F, Picano E: Occupational Health Risks in Cardiac Catheterization Laboratory Workers. Circ Cardiovasc Interv 2016, 9(4):e003273.
4. Lalabekyan B, Rennie A, Luoma V: Principles of radiation safety for anaesthetists. BJA Education 2025, 25(5): 181e190.