Postoperative Apnea and Former Preterm Infant: Evolving Evidence for Management
Myron Yaster MD, Priti G. Dalal MD, Charles J. Coté MD
Today’s PAAD comes from the June 2025 issue of the Anesthesia Patient Safety Foundation Newsletter.1 The article is a quick read, indeed, not much longer than this PAAD, so, I’d urge all of you to read it in its entirety, discuss it with your colleagues, and use it as a teaching tool in the OR. I’ve asked 2 of the authors of the article, Drs. Charlie Coté and Priti Dalal, to join me in writing today’s PAAD. As many of you know, Charlie has been researching this issue for decades and Priti has more recently championed it via Wake Up Safe and the Society for Pediatric Anesthesia’s Quality and Safety Committee. Finally, although the issues discussed in the article are important to every practicing pediatric anesthesiologist, it is especially important to anyone preparing for their Anesthesiology and Pediatric Anesthesiology Board examinations! Myron Yaster MD
Original article
Ying Eva Lu-Boettcher, MD; Rahul Koka, MD, MPH; Priti G. Dalal, MD; Charles J. Coté, MD; Members of Wake Up Safe/Society of Pediatric Anesthesia Quality & Safety committee. Postoperative Apnea and Former Preterm Infant: Evolving Evidence for Management, Anesthesia Patient Safety Foundation, June 2025 https://www.apsf.org/article/postoperative-apnea-and-former-preterm-infant-evolving-evidence-for-management/?utm_source=APSF+Newsletter+Email+-+External&utm_medium=email&utm_campaign=EMAIL_CAMPAIGN_2025_06_01
“Preterm” (< 37 weeks gestational age) and former preterm infants are known to be at increased risk for postoperative apnea following emergence from anesthesia.”2-4 Please note: In most studies cited in today’s PAAD, post conceptual age is used to define an infant’s age. This term, post-conceptual age, is now discouraged; “Post menstrual age (completed weeks) is now preferred by the American Academy of Pediatrics. As a reminder (see PAAD 02/05/2025 https://ronlitman.substack.com/p/remembering-the-classics-how-old ): Post menstrual age is the time elapsed between the first day of the last menstrual period and the day of delivery. If pregnancy was achieved using assisted reproductive technology, gestational age is calculated by adding 2 weeks to the conceptional age.”5
How is apnea defined? Why are newborns at increased risk? And when is the risk reduced? “Apnea of prematurity is defined as a respiratory pause for more than 15–20 seconds, or shorter respiratory pauses accompanied by oxygen desaturation or bradycardia (heart rate < 100 beats per minute, or <20% from baseline) in preterm and former preterm infants.”1,6 It occurs because the newborn has immature control of ventilation and responds to hypoxemia and hypercarbia (immature peripheral and central chemoreceptors) with periodic breathing, hypoventilation, apnea and bradycardia rather than tachypnea and tachycardia.1,7
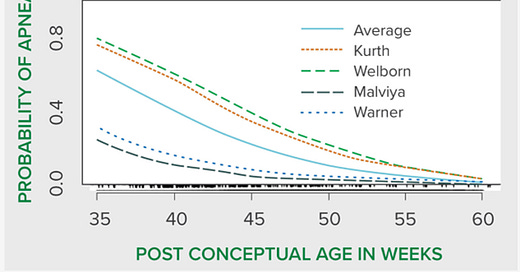
Aside from the risk of apnea in former premature infants in general, the risk is further increased following anesthesia (post operative apnea) because airway obstruction is so common after an anesthetic, particularly a general anesthetic, and because residual effects on respirations (a combination of central and obstructive apnea). The risk for postoperative apnea is inversely related to gestational age and increases with cardiac shunts, anemia, decreasing post conceptual age at time of surgery, hypothermia, glucose and electrolyte disturbances, and a patent ductus arteriosus.1,4
Thus, when anesthetizing a newborn what should you do? The authors provide a wonderful figure and chart reproduced below:
Although it is hard to find case reports of post-operative apnea in former preterm infants less than 60 weeks or even greater than 60 weeks PMA in the current available literature, a detailed analysis of raw data from existing studies may identify the at-risk period for post-operative apnea in former preterm infants. So how should these patients be monitored? The authors recommend: “Apnea and bradycardia monitoring, nursing observation, continuous pulse oximetry, and a respiratory monitor.”1 I (MY) would add that this is best accomplished in a high surveillance unit (ICU or PACU) AND this monitoring should be used in transport from the OR to the PACU and when the patient is transferred to the wards.
Finally, today’s article does not discuss awake spinal anesthesia or neuraxial anesthesia. The late great Dr. Chris Abajian championed the use of awake spinal anesthesia for surgery in these high risk patients and felt that it was much safer than general anesthesia.8 Unfortunately, although the risk of apnea is reduced when using awake spinal anesthesia it is not eliminated and cardiorespiratory monitoring post operatively is still required.9
Send your thoughts and comments to Myron who will post in a Friday reader response.
References
1. Lu-Boettcher YE, Koka R, Dalal PG, Coté CJ: Postoperative Apnea and Former Preterm Infant: Evolving Evidence for Management, Anesthesia Patient Safety Foundation, 2025
2. Cote CJ, Zaslavsky A, Downes JJ, Kurth CD, Welborn LG, Warner LO, Malviya SV: Postoperative apnea in former preterm infants after inguinal herniorrhaphy. A combined analysis [see comments]. Anesthesiology 1995; 82: 809–822
3. Kurth CD, Spitzer AR, Broennle AM, Downes JJ: Postoperative apnea in preterm infants. Anesthesiology 1987; 66: 483–488
4. Zhao J, Gonzalez F, Mu D: Apnea of prematurity: from cause to treatment. Eur J Pediatr 2011; 170: 1097–105
5. Engle WA: Age terminology during the perinatal period. Pediatrics 2004; 114: 1362–4
6. Eichenwald EC: Apnea of Prematurity. Pediatrics 2016; 137
7. Erickson G, Dobson NR, Hunt CE: Immature control of breathing and apnea of prematurity: the known and unknown. J Perinatol 2021; 41: 2111–2123
8. Abajian JC, Mellish RW, Browne AF, Perkins FM, Lambert DH, Mazuzan JE, Jr.: Spinal anesthesia for surgery in the high-risk infant. Anesth.Analg. 1984; 63: 359–362
9. Davidson AJ, Morton NS, Arnup SJ, de Graaff JC, Disma N, Withington DE, Frawley G, Hunt RW, Hardy P, Khotcholava M, von Ungern Sternberg BS, Wilton N, Tuo P, Salvo I, Ormond G, Stargatt R, Locatelli BG, McCann ME: Apnea after Awake Regional and General Anesthesia in Infants: The General Anesthesia Compared to Spinal Anesthesia Study--Comparing Apnea and Neurodevelopmental Outcomes, a Randomized Controlled Trial. Anesthesiology 2015; 123: 38–54