Population Pharmacokinetics of Single Bolus Dose Fentanyl in Obese Children
Myron Yaster MD and Lynne G. Maxwell MD
As regular readers of the PAAD know, I’ve often said (PAAD, “obesity in adolescents”, August 16, 2023) that obesity is to this generation what smoking was to mine. The prevalence of pediatric obesity continues to increase and represents a significant international health crisis with profound implications for future life expectancy and health care spending. In the United States, the prevalence of obesity in 2015-2016 was 20.6% among adolescents (as compared with 14.8% in the 1999–2000 period) — 22.0% among non-Hispanic Black adolescents and 25.8% among Hispanic adolescents.1,2 And this is no longer an isolated American problem. Obesity is spreading throughout the world in high, middle, and low income countries.
When faced with an obese pediatric patient how should one dose intravenous drugs? In today’s PAAD3 and accompanying editorial,4 the authors looked at what happens to a single dose of fentanyl administered after the induction of anesthesia in obese and non-obese children presenting for adenotonsillectomy surgery. The fentanyl dosing in both groups was based on total body weight (TBW). Would TBW lead to excessive fentanyl plasma levels in obese children? Myron Yaster MD
Original article
Okada CR, Henthorn TK, Zuk J, Sempio C, Roosevelt G, Ruiz AG, Cohen MN, Chatterjee D, Galinkin JL. Population Pharmacokinetics of Single Bolus Dose Fentanyl in Obese Children. Anesth Analg. 2024 Jan 1;138(1):99-107. doi: 10.1213/ANE.0000000000006554. Epub 2023 Dec 15. PMID: 37801572.
Editorial
Ingrande J. Bolus Dose Administration of Fentanyl in Obese Children: Do Settle for Less. Anesth Analg. 2024 Jan 1;138(1):96-98. doi: 10.1213/ANE.0000000000006717. Epub 2023 Dec 15. PMID: 38100803.
“Typically in pediatric anesthesia, anesthetic medications are administered in accordance with a patient’s weight. There are many weight-based dosing scalars (total body weight, lean body weight, ideal body weight, body surface area, etc), and there are also many equations that exist for calculating some of these scalars. Confusion exists about which weight-based dosing scalar is best. In a patient of normal weight, the question of which dosing scalar to use is nonconsequential––a lean patient’s total body weight, lean body weight, and ideal body weight are all similar. But what about an obese patient? And what about pediatric patients, in whom medications have been scaled in accordance with body weight, body weight scaled allometrically, and body surface area?”4
Okada et al.3 administered a single fentanyl dose (1 mcg/kg) based on total body weight to 2-12 year old obese and non-obese patients anesthetized for elective tonsillectomy. The fentanyl was administered after a sevoflurane induction of anesthesia and the placement of 2 IV catheters, one for drug administration and the other for blood sampling.
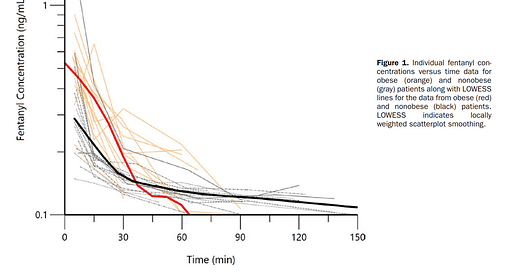
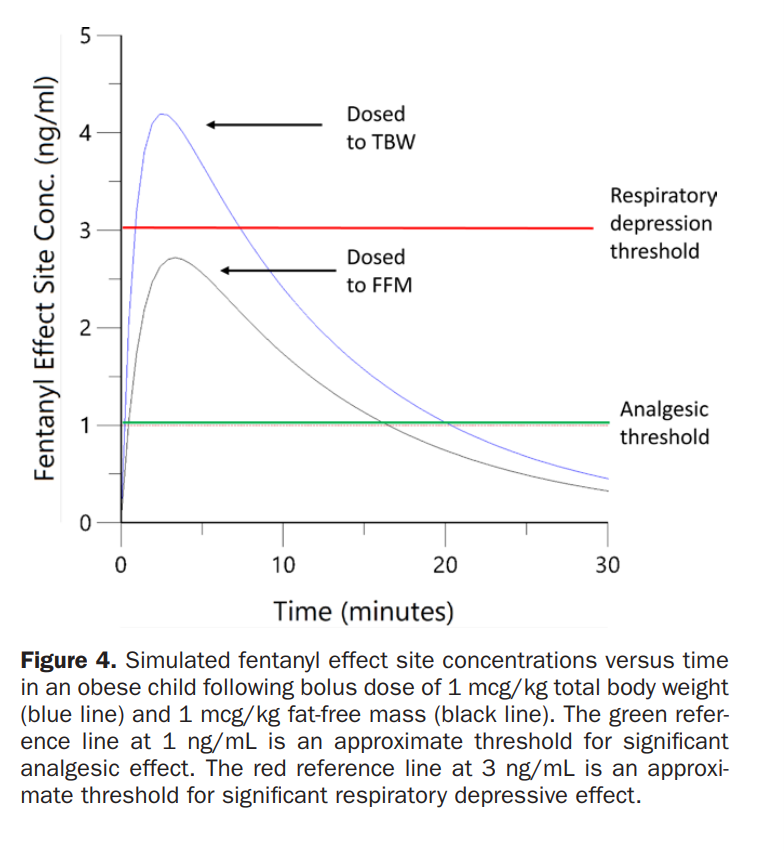
Not surprisingly, “higher peak plasma concentrations of fentanyl were found in obese children compared to their lean counterparts. Fat-free mass (FFM) (also known as lean body weight) was a significant covariate for the central volume of distribution.”3,4 Diving a little deeper, fentanyl is highly lipophilic and some people believed that a higher initial fentanyl dose based on total body weight would not produce higher blood levels because the fentanyl would be distributed to and trapped in fat and therefore not result in higher blood levels. However, in his editorial, Ingrade4 points out that this didn’t occur in the Okada et al. study probably because blood flow to fat is so poor, the volume of distribution is not increased in proportion to increased body weight. Thus, following a single bolus dose, the adipose tissue “plays an insignificant role in the early distribution kinetics of our anesthetics and thereby results in higher plasma concentrations of the drug.” Indeed, using total body weight instead of lean body weight, Okada et al. found that plasma concentrations exceeded the threshold for respiratory depression in the obese patients in their study (figures 1 and 2). It is important to note though, that in this small study, actual respiratory depression was not seen. Additionally, most of the non-obese patients required opioid supplementation in the PACU and the obese patients did not!
Based on Okada et al.’s study, initial fentanyl dosing should be based on lean body weight and not total body weight. One of the problems that I (MY) found when I was practicing clinical medicine was how to calculate lean body weight (or FFM) versus ideal body weight.5 An alternative and simple technique to use in the obese pediatric patient (BMI > 95 percentile, and I used this technique only if BMI was > 120 percentile) is to use allometric scaling.6 It doesn’t always work but it is clean and easy if you have an iphone, and these days who doesn’t? In allometric scaling the weight to use in your mg/kg or mcg/kg dosing is the patient’s actual total body weight raised to the square root of 0.75 (.86). For example, using your cell phone calculator turned horizontally to become a scientific calculator, find the xy function. Assuming a body weight of 150 kg, then X = 150 (kg) and the y constant = 0.86… resulting in a scaled weight of 74.4 kg.
What do you do in your practice? Send your thoughts and tricks to Myron who will post in a Friday reader response.
References
1. Hannon TS, Arslanian SA. Obesity in Adolescents. New England Journal of Medicine 2023;389(3):251-261. DOI: 10.1056/NEJMcp2102062.
2. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS data brief 2020(360):1-8. (In eng).
3. Okada CR, Henthorn TK, Zuk J, et al. Population Pharmacokinetics of Single Bolus Dose Fentanyl in Obese Children. Anesthesia and analgesia 2024;138(1):99-107. (In eng). DOI: 10.1213/ane.0000000000006554.
4. Ingrande J. Bolus Dose Administration of Fentanyl in Obese Children: Do Settle for Less. Anesthesia and analgesia 2024;138(1):96-98. (In eng). DOI: 10.1213/ane.0000000000006717.
5. Anderson BJ, Holford NH. Getting the dose right for obese children. Archives of disease in childhood 2017;102(1):54-55. (In eng). DOI: 10.1136/archdischild-2016-311696.
6. Holford NHG, Anderson BJ. Allometric size: The scientific theory and extension to normal fat mass. European Journal of Pharmaceutical Sciences 2017;109:S59-S64. DOI: https://doi.org/10.1016/j.ejps.2017.05.056.