Physician burn out part 1
Myron Yaster MD, Amy Benedikt MD, Illana Fromer MD, Rebecca Margolis DO, and Norah Janosy MD
The entire issue of Anesthesiology Clinics (Volume 40 issue 2) is devoted to physician health, well-being, quality of life, and burnout, topics that we’ve addressed in the PAAD before. I’ve asked several members of SPA’s Well-Being Committee to assist me in the reviews of some of these articles which I will post over the next 2 months. First and foremost, I and many of you, are getting burned-out by burn out articles and institutional policies that blame you the victim for these problems. Thus, what I will not do in these forthcoming PAADs is to recount the BS of mandatory resiliency modules, programs that tick off check boxes for hospital/departmental leaders and administrators to blame the victims (you) rather than implementing structural change, or think that free pizza and “retreats” will fix these problems. (I must also admit that I (and the late legendary general George S. Patton) hate the idea of “retreats”…we prefer “advance”!)
I’m going to pick articles from this issue that have evidence-based solutions. I’ve asked the leaders of SPA’s Well-Being committee and their communication working group to help me with these reviews and I’ve asked them to become regular contributor/reviewers for the PAAD. This is a relatively new SPA committee, chaired by Rebecca Margolis and Norah Janosy. Its goals (from the website) are “to promote a culture of emotional, physical, and psychological well-being amongst SPA members by providing resources, support, and connections. The SPA Well-Being Committee will act as the focal point for wellness efforts directed at the SPA membership via annual meeting program content, workshops, and leadership development”. Like all SPA committees they are open to anyone with an interest to join. You don’t have to be asked or appointed…just show up and/or contact Rebecca and Norah. Myron Yaster MD
Original article
Sinskey JL, Chang JM, Nicholau D, Gropper MA. Quality of Life Improvement: A Novel Framework and Approach to Well-Being. Anesthesiol Clin. 2022 Jun;40(2):415-432. PMID: 35659411
“While there is increasing awareness of the importance of systems approaches to combat burnout and foster physician well-being, few tools exist for organizations to operationalize the concept of well-being in the clinical setting. Abstract discussions of well-being without concrete action can paradoxically contribute to burnout by eroding physicians’ trust in leadership and the institution”.1 This article reviews techniques used in Quality improvement (QI) and implementation science (IS) to propose methods for quality of life improvement”.1
There were two key points in this article that we found especially meaningful in helping to improve our mental health. One is that quality of life improvement needs to be addressed on both the individual and systems levels. Keeping that in mind, the authors then lay out a detailed approach to make that happen, which is our second favorite thing about the article.
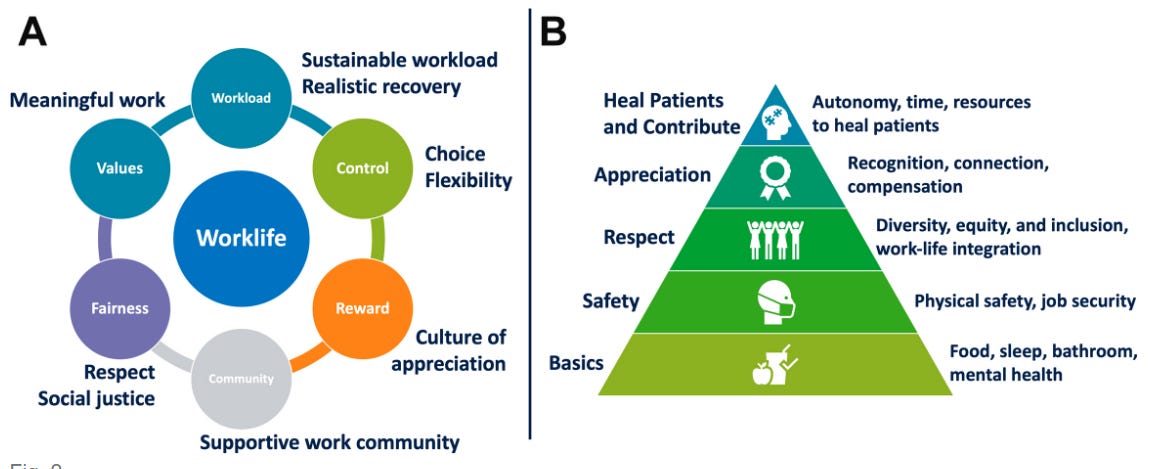
“A clear structural framework can promote a consistent approach to thinking about clinician well-being. Two such frameworks are (1) the 6 areas of worklife model proposed by Leiter and Maslach and (2) a modified Maslow’s hierarchy of physician burnout and wellness needs.2,3 “The areas of worklife model provides an organizational context of burnout by identifying areas of worklife whereby the degree of mismatch between a person and their work is predictive of burnout. These areas are workload, control, reward, community, fairness, and values. This framework allows institutions to develop tailored initiatives to improve matches in these 6 areas. An assessment of clinicians’ satisfaction within the 6 areas can provide valuable information to design a well-being strategy that builds on existing strengths while targeting key stressors in the work environment”.1
To be honest, this is where my eyes glaze over and I (MY) lose consciousness faster than if I was given propofol. For me (AB), the first thing I thought of when I looked at the pyramid was the healthy food pyramid. Knowing that our basic needs are taken care of, we can then move up the pyramid. Check out the base of the pyramid which includes our mental health- that’s how important it is. What I (MY) want to know is, what are the solutions? The authors borrow from six/lean sigma, quality improvement and implementation science for improvement: “(1) early stakeholder engagement to identify the correct problem, (2) a collaborative approach, and (3) continuous and rapid prototyping”.1
For those of you who are not as familiar with six sigma: “QI embodies the idea that the system and infrastructure, and not the individual, should be the focus of efforts to improve the quality of care and prevent future harm. Therefore, QI efforts emphasize system issues rather than individual shortcomings in an ongoing process of reassessment, readjustment, and continuous improvement. QI is characterized by a rigorous feedback process which includes systematically defining and evaluating metrics to determine whether improvement efforts lead to intended changes and ensure that there are no unintended negative consequences. Implementation science is the systematic study of how to design and evaluate a set of activities to facilitate the successful uptake of an evidence-based health intervention”.1
This approach can be summarized by 3 questions: “ (I) why is this problem important, (II) what are we going to do about it, and (III) how do we keep improving?”1
We can all agree it’s a problem. For the rest of this review, let’s zero in on “what are we going to do about it?” The authors recommend that after setting up the team, focus and prioritize practical solutions that will work. As in six/lean sigma, the “PICK (Possible, Implement, Challenge, and Kill) tool is used to prioritize QI efforts by assessing ease of implementation and level of payoff. Well-being initiatives that fall in the “Implement” category should be prioritized first, followed by “Possible,” which represent quick wins. Creating a plan for “Challenge” initiatives can help build a long-term strategy. Initiatives in the “Kill” category should not be pursued further.
The example of a Kill category presented by the authors involve trying to get people out of the ORs on time at the end of the day, with a solution that prevents elective surgery after say 3 or 4 PM. It may work, but will not have any institutional or support by the surgeons. So, although a good idea it can’t be successfully implemented and needs to be dropped/killed. On the other hand, the authors instituted an “early leave” and late start where some faculty came in late and stayed longer and others started early and left early. The institution and department bought into this and it worked well with modifications along the way. As they reviewed this they realized it didn’t work in July and August when the pediatric ORs are at the busiest and the new residents could not function independently.
In order to implement this program, the authors describe in detail what is required. The strategies include building a team, assessing the landscape, defining the problem, evaluating the metrics, and iterating.
Could this process work in your institution and practice? Do you have the time and resources to make it happen? Continuing to do what we know doesn’t work is the definition of insanity. This article presents a framework that offers solutions which requires incredible commitment and buy-in from your department and all of it’s members. Wouldn’t it be incredible if physician mental health became a priority within our departments/hospital systems? Resources to help are available at the ASA and SPA websites. In future PAADs we will provide these links to you.
References
1. Sinskey JL, Chang JM, Nicholau D, Gropper MA: Quality of Life Improvement: A Novel Framework and Approach to Well-Being. Anesthesiol Clin 2022; 40: 415-432
2. Maslach C, Leiter MP: New insights into burnout and health care: Strategies for improving civility and alleviating burnout. Med Teach 2017; 39: 160-163
3. Shapiro DE, Duquette C, Abbott LM, Babineau T, Pearl A, Haidet P: Beyond Burnout: A Physician Wellness Hierarchy Designed to Prioritize Interventions at the Systems Level. Am J Med 2019; 132: 556-563