Guidelines, Guidelines everywhere…Is optimal cardiac arrest care determined by continent? Part 2
Myron Yaster MD, Justin L. Lockman MD MSEd, Jayant K. Deshpande MD
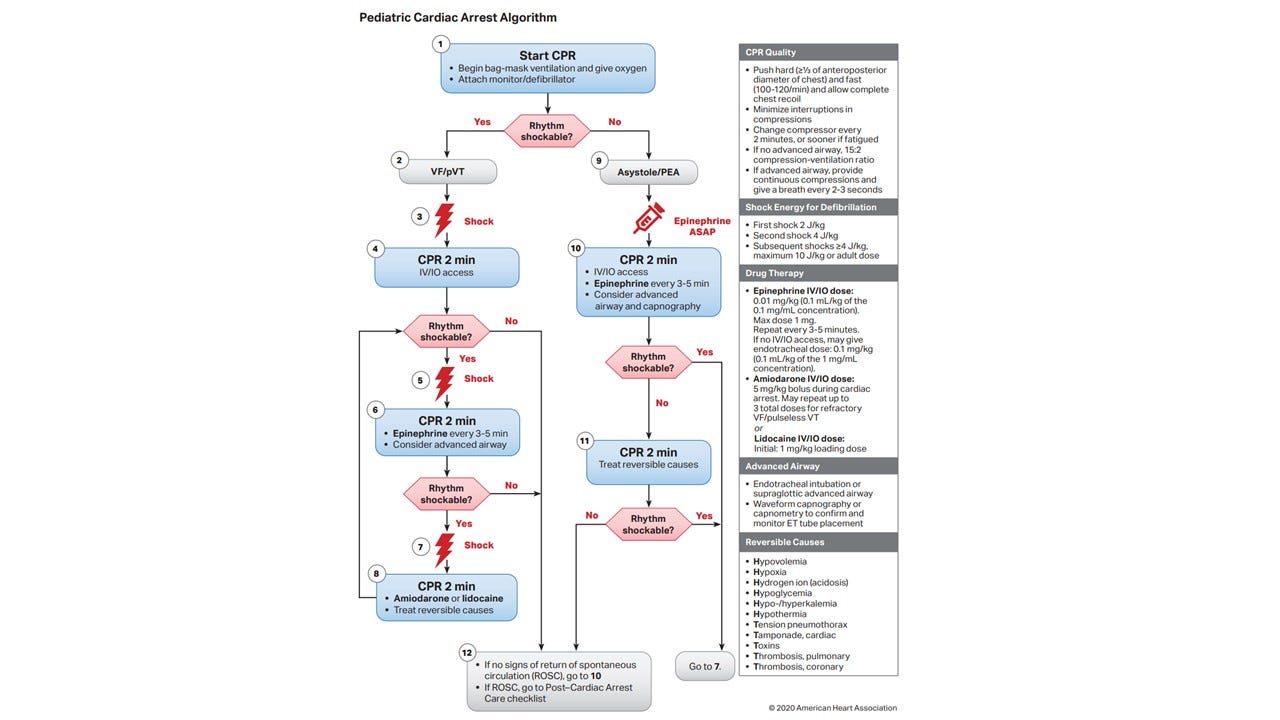
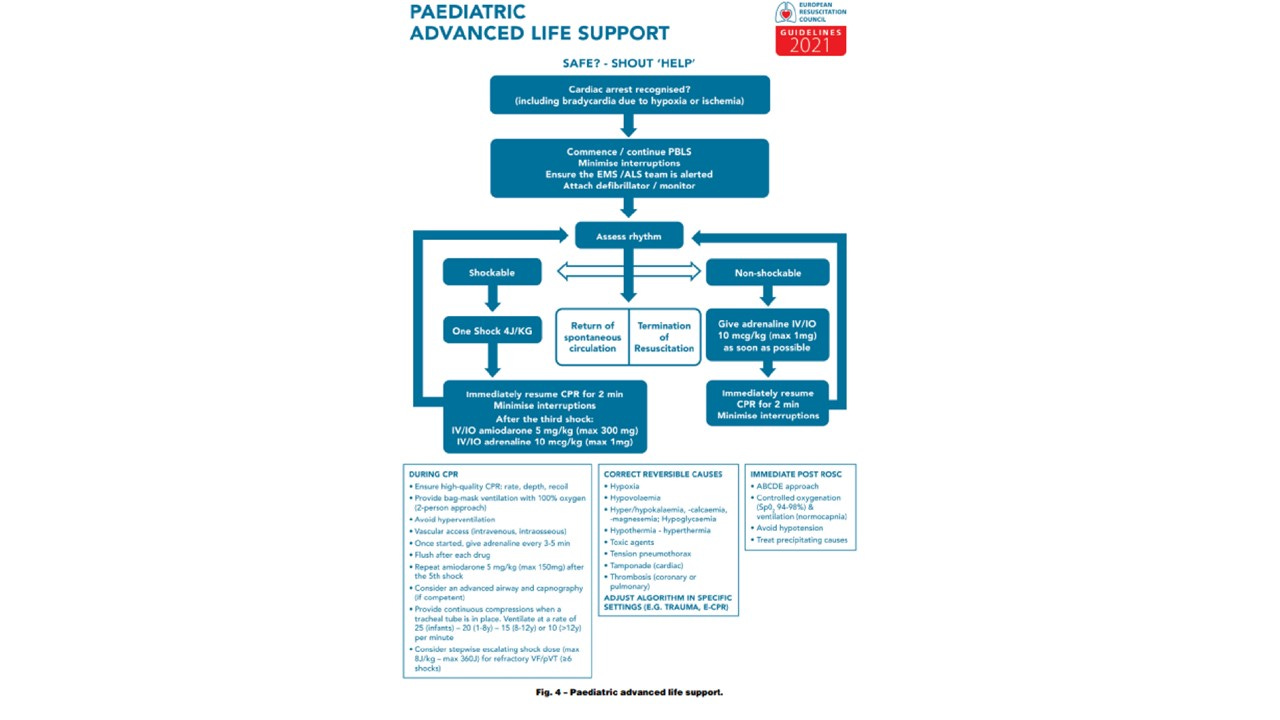
In yesterday’s PAAD, we described the development of the Society for Pediatric Anesthesia’s PediCrisis app and how the committees involved in its construction deliberately chose to align the content with the American Heart Association’s PALS guidelines. (if you haven’t downloaded this app on your cell phone do it NOW by clicking here! ). These guidelines are often in sync with guidelines from other Societies but not always. Yesterday we discussed drug calculation tools and rules, atropine, oxygen therapy, ventilation strategies, and fluid therapy. In today’s part 2 of the PAAD, we will review vaso-active drugs, Tranexamaic Acid (TXA), tension pneumothorax, and stacked shocks and energy dose for shocking the heart highlighting some of the differences of the new European Resuscitation guidelines. Myron Yaster MD
Original article
Buis ML, Turner NM. New European Resuscitation Council guidelines for pediatric life support and their implications for pediatric anesthesia: An educational article. Paediatr Anaesth. 2022 Apr;32(4):497-503. PMID: 34964208
Vasoactive drugs In the European guidelines, there are choices of EPINEPHRINE or NOREPINEPHRINE and avoidance of DOPAMINE. Additionally, the inodilator MILRINONE is suggested for patients with cardiac dysfunction. In PediCrisis we only recommend boluses of EPINEPHRINE 10 MICROgrams/kg q3 minutes and if no ROSC, consider rapidly activating ECMO if available (and again this harnesses the power of the cell phone!). Interestingly, milrinone and norepinephrine may have some value, particularly after ROSC. We currently do not have a checklist for post-resuscitation care in the Cardiac Arrest checklist or the app. Should we add this in the future? We also agree with doing away with dopamine once and for all – it’s a “dirty” drug with lots of side effects, and there are better options. What do you think?
Tranexamic Acid (TXA); the European guidelines advocate TXA in severe trauma and/or massive hemorrhage. They recommend A loading dose of 15–20 mg/kg (max. 1 gram) followed by a continuous infusion of 2 mg/kg/hour for at least 8 hours or until the bleeding stops. There are many other TXA cocktails. We do not have a TXA recommendation in our massive hemorrhage event list and we couldn’t find this recommendation in the AHA PALS guidelines. Should we add it to the app?
Tension pneumothorax. The European guidelines state that the preferred site for needle decompression of a tension pneumothorax is the 4th or 5th intercostal space (ICS) slightly anterior to the midaxillary line. This is also consistent with updated ATLS (Advanced Trauma Life Support) guidelines. In the PediCrisis app we recommend rapid decompression by placing a needle in the 2nd rib space mid-clavicular line, which was the historically-taught method. The app also recommends placing a chest tube in the 5th-6th intercostal space mid axillary line. We’ve discussed this important difference in the last checklist committee meeting without changing our recommendations. Perhaps we need to add this again to our next agenda?
Stacked shocks and energy dose for shocks: The standard energy dose remains 4 J/kg in both the app and the new European guidelines. In the app we do not recommend maximum energy doses because recommended maximum doses vary with defibrillator manufacturer and type: for biphasic defibrillators, the maximum dose is usually between 120 and 200 joules; for monophasic defibrillators, the maximum dose is usually 360 joules. If more than 5 shocks are needed for refractory VF/pulseless VT, escalating doses of up to 8 J/kg are recommended in the app. The European and AHA PALS guidelines recommend going up to a max of 10 J/kg. the European guidelines also suggest, “despite very limited evidence, we advise using a ‘stacked’ shock approach for those children who are monitored and have a defibrillator immediately ready for use at the moment of a ‘witnessed’ VF/pVT.” The stacked approach is back-to-back defibrillation up to 3 doses, with the hope of establishing a perfusing rhythm. This was historically recommended in AHA guidelines as well but was taken out due to delays in chest compressions during the stacked shocks. Most recently, while advocating for early defibrillation in the event VT, the 2020 AHA guidelines and the PediCrisis app do not recommend delaying chest compressions or further treatment in order to provide initial defibrillation, and stacking shocks at the cost of holding compressions is doing just that in our view. What do you think?
We’ve raised a lot of issues in these PAADs. Please let us know your thoughts (send directly to my email: myasterster@gmail.com) and we’ll post in a future reader response. Finally, please remember that ALL SPA committees are open for any member to join. If you are interested in checklists, the app, information technology, quality and safety please take this opportunity to join! Just go to the website.
Myron Yaster MD, Justin L. Lockman MD MSEd, Jayant K. Deshpande MD