Otitis media is one of the most frequently diagnosed infectious diseases in children1 and insertion of tympanostomy tubes (aka PE tubes, or pressure equalization tubes) to treat “persistent middle ear fluid, frequent ear infections, or ear infections that persist after antibiotic therapy”2 is the most common ambulatory surgery performed on children in the United States. I’m certain that everyone reading the PAAD has provided anesthesia for tympanostomy tubes (plus minus adenoidectomy and tonsillectomy). When I read the article by Shaikh in the New England J of Medicine, I thought it would be a great refresher course for many of you on the etiology and treatment of acute otitis media. I also included a recent clinical practice guideline on PE tubes as well which we will review with some of our otolaryngologist colleagues at a future date. Myron Yaster MD
Original article
Shaikh N. Otitis Media in Young Children. N Engl J Med. 2025 Apr 10;392(14):1418-1426. doi: 10.1056/NEJMcp2400531. PMID: 40214033.
Original article
Rosenfeld RM, Tunkel DE, Schwartz SR, Anne S, Bishop CE, Chelius DC, Hackell J, Hunter LL, Keppel KL, Kim AH, Kim TW, Levine JM, Maksimoski MT, Moore DJ, Preciado DA, Raol NP, Vaughan WK, Walker EA, Monjur TM. Clinical Practice Guideline: Tympanostomy Tubes in Children (Update). Otolaryngol Head Neck Surg. 2022 Feb;166(1_suppl):S1-S55. doi: 10.1177/01945998211065662. PMID: 35138954.
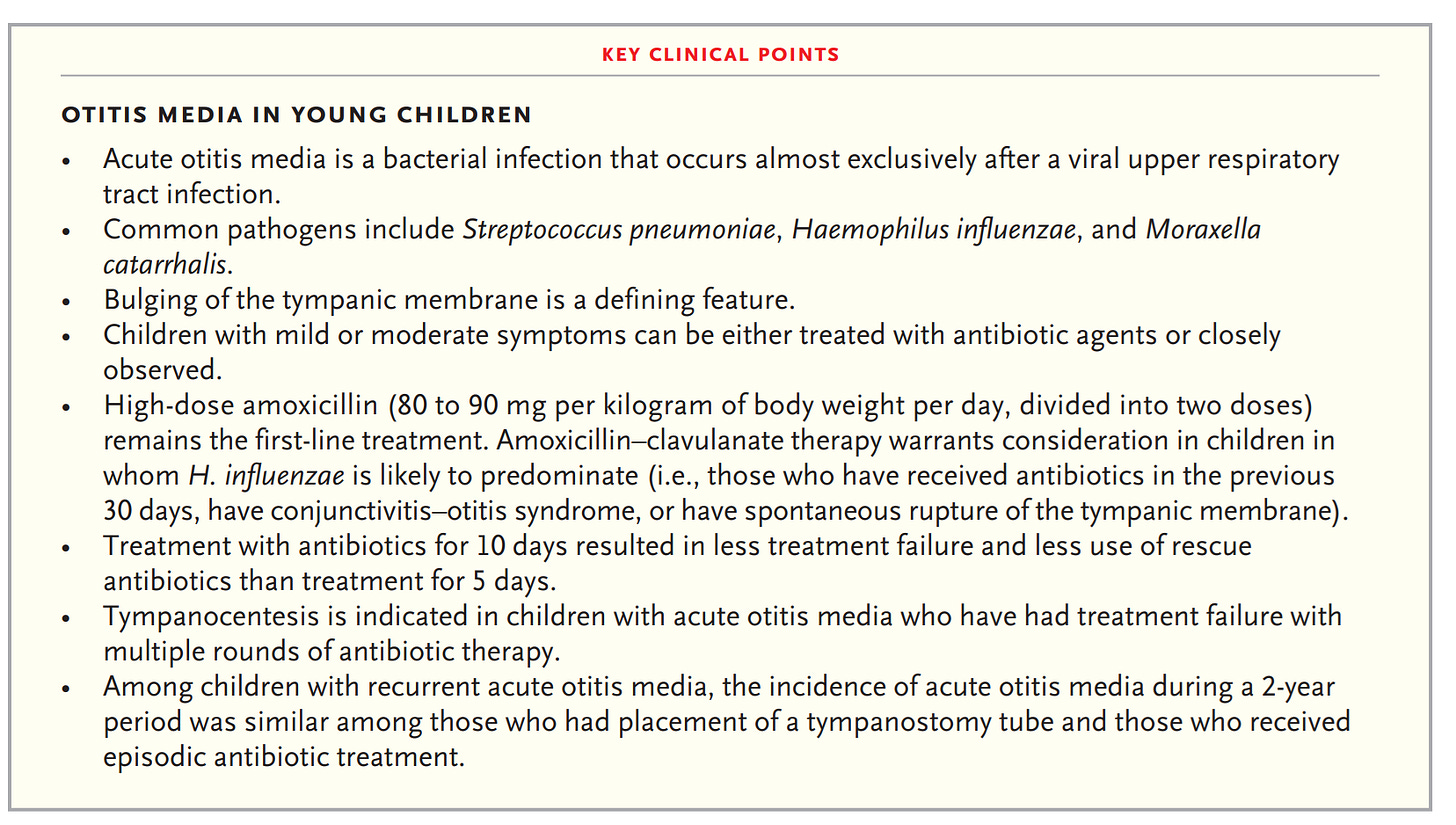
Pretty much every kid less than 2 years of age gets at least one ear infection. Some, particularly those exposed to many other children (think day care) get many. Other risk factors for increased number of infections include male sex, children who experienced shorter duration of breast feeding, tobacco smoke exposure, Down syndrome and immunologic deficiencies (hypogammaglobinemia). “The antecedent event in almost all cases of acute otitis media is a symptomatic viral upper respiratory tract infection. Approximately one third of viral upper respiratory tract infections are complicated by acute otitis media. Viral infection inflames the mucosa of the upper respiratory tract, including the nasopharynx and eustachian tube. Eustachian-tube dysfunction impairs the drainage of fluid from the middle ear and leads to nasopharyngeal aspiration of pathogens. Bacteria (most often Streptococcus pneumoniae, nontypable Haemophilus influenzae, and Moraxella catarrhalis) are isolated from the middle-ear fluid of approximately 80% of children with a bulging tympanic membrane.”1 The incidence of acute otitis media is decreasing and is “attributable to universal vaccination with pneumococcal conjugate vaccines and to increased stringency in the diagnostic criteria.”1 Treatment is with antibiotics. The key clinical points from the article are in the figure/table below.
“Recurrent acute otitis media is conventionally defined as three or more episodes occurring within 6 months or as four or more episodes occurring within 12 months. Children with recurrent acute otitis media often undergo placement of a tympanostomy tube. The efficacy of tympanostomy-tube placement in the prevention of recurrences of acute otitis media has been evaluated in six trials. In the largest and most recent trial, the incidence of acute otitis media during a 2-year follow-up period was similar among children who underwent tympanostomy tube placement and those who received episodic antibiotic treatment.3”1
Send your thoughts and comments to Myron who will post in a Friday reader response.
References
1. Shaikh N. Otitis Media in Young Children. The New England journal of medicine 2025;392(14):1418-1426. (In eng). DOI: 10.1056/NEJMcp2400531.
2. Rosenfeld RM, Tunkel DE, Schwartz SR, et al. Clinical Practice Guideline: Tympanostomy Tubes in Children (Update). Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2022;166(1_suppl):S1-s55. (In eng). DOI: 10.1177/01945998211065662.
3. Hoberman A, Preciado D, Paradise JL, et al. Tympanostomy Tubes or Medical Management for Recurrent Acute Otitis Media. The New England journal of medicine 2021;384(19):1789-1799. (In eng). DOI: 10.1056/NEJMoa2027278.