Guidelines, Guidelines everywhere…Is optimal cardiac arrest care determined by continent? Part one
Myron Yaster MD, Justin Lockman MD MSEd, Jayant K Deshpande MD
In my opinion, one of the most important achievements of the Society for Pediatric Anesthesia was the development and distribution of the Society’s PediCrisis app (version 2) and the checklists for critical OR events that were the basis for the app. Before going any farther, if you haven’t downloaded this app on your cell phone do it NOW by clicking here! An updated version 3 of the app should be released any day now (I hope!). The new version will allow the user to pick a language (English or Spanish) and has been updated based on the recommendations of SPA’s Quality and Safety Committee and the Checklist and App subcommittees. We all owe a huge debt of gratitude to all who worked on these projects and to its leaders, Drs. Priti G. Dalal, Anna Clebone, Kim Strupp and Barbara Burian for their tireless work in keeping these projects moving forward and up to date. Additionally, we also owe a debt of gratitude to Drs. Genie Heitmiller and Don Tyler who were instrumental in the creation of these committees and to the CHOP team (Drs. Galvez, Schleelein, Rehman, Lockman, and others) who developed version 1 of the app.
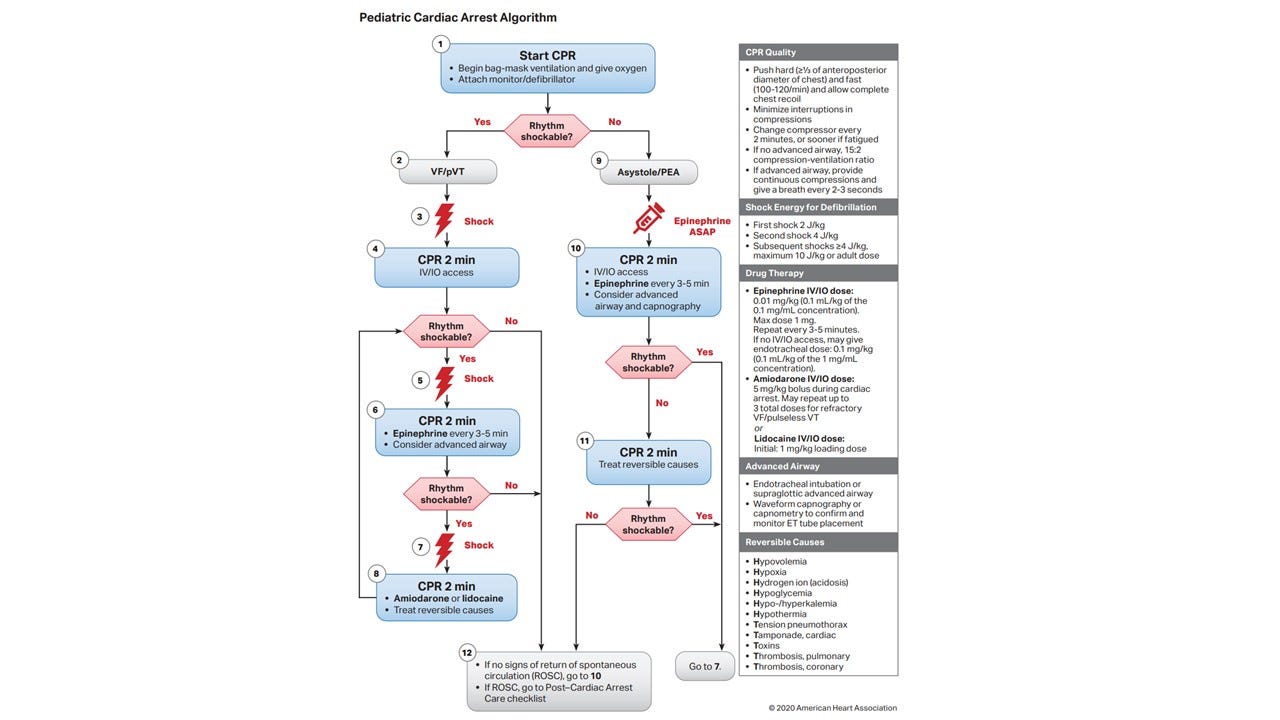
In developing the Critical Events Checklists (which you can find here) and the PediCrisis app, the committees involved in their construction deliberately chose to align the content with the American Heart Association’s PALS/APLS guidelines (Figure 1). These guidelines are often in sync with guidelines from other Societies but not always. In today’s PAAD, we highlight some of the differences of the new European Resuscitation guidelines (Figure 2) for pediatric advanced life support and their implications.1 I’ve asked Justin Lockman and Jay Deshpande to write this with me AND I ran some of the issues raised in today’s article by SPA’s checklist leaders Drs. Priti Dalal and Anna Clebone as well. Finally, simply because of the sheer volume of information to discuss, I’ve split today’s PAAD into 2 parts. Part 2 will appear tomorrow. Myron Yaster MD
Original article
Buis ML, Turner NM. New European Resuscitation Council guidelines for pediatric life support and their implications for pediatric anesthesia: An educational article. Paediatr Anaesth. 2022 Apr;32(4):497-503. PMID: 34964208
“Rates of survival to hospital discharge in children with in-hospital cardiac arrests have improved over the past decade without higher rates of neurological disability among survivors”.2 Preventing delays in initiating CPR and adherence to published guidelines is crucial in this survival improvement.3,4 Today’s article takes a novel approach in presenting the new European resuscitation guidelines. Instead of presenting lists and algorithms, it presents the illustrative case of an 11-month-old with acute renal failure who presents for placement of a central venous dialysis catheter in the OR…and the child arrests during the procedure. What to do? What to do?
Drug calculation tools and rules. Fortunately, in the OR we usually have accurate weights. But can we rely on our ourselves or team to make drug calculations accurately during a crisis? One of the great things about the PediCrisis app is that utilizes the power of your cell phone. If you enter the patient’s weight into the crisis checklist, the app will make the calculations for you. Additionally, because it is a cell phone, if you have prepopulated the app’s phone directory at the time of app download or any time thereafter, by simply tapping the phone, it will call the appropriate phone numbers that you may need during a crisis (e.g., OR front desk/overhead, pharmacy, blood bank, ECMO, etc.).
Atropine: Even though many pediatric anesthesiologists still pick up a syringe of atropine to treat bradycardia almost reflexively, the use of atropine in pediatric resuscitation remains a matter of controversy. Indications for its use include vagally-induced bradycardia, prior to use of succinylcholine for endotracheal intubation, organophosphate toxicity (and maybe some other toxidromes) and possibly atrioventricular block. In the setting of acute deterioration of an infant or child, the precise etiology of the bradycardia may be unclear and the use of atropine is not unreasonable. The 2020 AHA PALS algorithm for pediatric bradycardia includes atropine. While this algorithm also states a minimum dose of atropine, there is little evidence to substantiate this. However, in the unstable bradycardic patient, EPINEPHRINE, not atropine, should be the first syringe you pick up.
Oxygen Therapy “Compared with the previous guideline, more emphasis is placed on the avoidance of hyperoxia, based on evidence of its deleterious effects following ROSC [Return Of Spontaneous Circulation]”.5 The PediCrisis app recommends an FiO2 of 1.0 during cardiac arrest. Perhaps we should change this to start with an FiO2 of 1.0 and titrate downward to a SpO2 of 94-98%? Perhaps this is not applicable in the perioperative setting? It’s tough since hypoxemia is a cause of some pediatric perioperative arrests and bradycardia. What is clear is that after ROSC there is usually no need and a clear risk for prolonged hyperoxia.
Ventilation strategy. The PediCrisis app recommends 10 breaths/minute during cardiac arrest. Updated PALS guidelines recommend a higher rate (range 20-30 breaths/minute) for infants and children The new European guidelines recommend variable, age-dependent rates: For infants, 25 breaths/ minute, for children between 1- 8 years, 20 breaths/minute. Would higher rates improve survival?6 We understand the rationale for the higher rate for children among both sets of guidelines, but worry that asking people to change strategy for different aged children (as in the European guidelines) may add to confusion during an already chaotic crisis.
In tomorrow’s PAAD, we will review fluid therapy, vaso-active drugs, Tranexamaic Acid (TXA), tension pneumothorax, and stacked shocks and energy dose for shocking the heart.
We’ve raised a lot of issues in today’s PAAD. Please let us know your thoughts (send directly to my email: myaterster@gmail.com) and we’ll post in a future reader response.
Myron Yaster MD, Justin Lockman MD MSEd, Jayant K Deshpande MD
References
1. Buis ML, Turner NM: New European Resuscitation Council guidelines for pediatric life support and their implications for pediatric anesthesia: An educational article. Paediatr Anaesth 2022; 32: 497-503
2. Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS: Survival trends in pediatric in-hospital cardiac arrests: an analysis from get with the guidelines-resuscitation. Circ.Cardiovasc.Qual.Outcomes. 2013; 6: 42-49
3. Buyck M, Shayan Y, Gravel J, Hunt EA, Cheng A, Levy A: CPR coaching during cardiac arrest improves adherence to PALS guidelines: a prospective, simulation-based trial. Resusc Plus 2021; 5: 100058
4. Bircher NG, Chan PS, Xu Y: Delays in Cardiopulmonary Resuscitation, Defibrillation, and Epinephrine Administration All Decrease Survival in In-hospital Cardiac Arrest. Anesthesiology 2019; 130: 414-422
5. Marquez AM, Morgan RW, Ko T, Landis WP, Hefti MM, Mavroudis CD, McManus MJ, Karlsson M, Starr J, Roberts AL, Lin Y, Nadkarni V, Licht DJ, Berg RA, Sutton RM, Kilbaugh TJ: Oxygen Exposure During Cardiopulmonary Resuscitation Is Associated With Cerebral Oxidative Injury in a Randomized, Blinded, Controlled, Preclinical Trial. J Am Heart Assoc 2020; 9: e015032
6. Sutton RM, Reeder RW, Landis WP, Meert KL, Yates AR, Morgan RW, Berger JT, Newth CJ, Carcillo JA, McQuillen PS, Harrison RE, Moler FW, Pollack MM, Carpenter TC, Notterman DA, Holubkov R, Dean JM, Nadkarni VM, Berg RA: Ventilation Rates and Pediatric In-Hospital Cardiac Arrest Survival Outcomes. Crit Care Med 2019; 47: 1627-1636
7. Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL Jr, Lasa JJ, Lavonas EJ, Levy A, Mahgoub M, Meckler GD, Roberts KE, Sutton RM, Schexnayder SM; Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020 Oct 20;142(16_suppl_2):S469-S523. doi: 10.1161/CIR.0000000000000901. Epub 2020 Oct 21. PMID: 33081526.
8. Van de Voorde P, Turner NM, Djakow J, de Lucas N, Martinez-Mejias A, Biarent D, Bingham R, Brissaud O, Hoffmann F, Johannesdottir GB, Lauritsen T, Maconochie I. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation. 2021 Apr;161:327-387. doi: 10.1016/j.resuscitation.2021.02.015. Epub 2021 Mar 24. PMID: 33773830.