Neonatal Video Laryngoscopy - Where Are We Now and Where Should We Go from Here?
Matthew J Rowland MD, Ethan Sanford MD, Shawn Jackson MD PhD
.Original Article
Bai W, Koppera P, Yuan Y, Mentz G, Pearce B, Therrian M, Reynolds P, Brown SES. Availability and Practice Patterns of Videolaryngoscopy and Adaptation of Apneic Oxygenation in Pediatric Anesthesia: A Cross-Sectional Survey of Pediatric Anesthesiologists. Paediatr Anaesth. 2025 Jun;35(6):460-468. doi: 10.1111/pan.15079. Epub 2025 Feb 5. PMID: 39907265; PMCID: PMC12060081.
Every few months, it seems like a new article is published demonstrating the superiority of video laryngoscopy (VL) to direct laryngoscopy (DL). This shouldn’t be surprising. VL provides “better glottic visualization, higher first‐attempt success, and fewer airway‐related complications.”1 Over the last year alone, we have read about the advantages of VL in the delivery room2 and in post cardiac arrest care.3 The European Society of Anesthesiologist and Intensive Care and British Journal of Anaesthesia joint guidelines recommend VL as first line in neonatal intubation and when a difficult airway is anticapated.4 Similarly, apneic oxygenation has shown promise in allowing increased time for intubation and reducing the risk of hypoxemia while intubating.5,6 It is recommended in all neonatal intubations by the same joint guidelines.4 Despite increasingly compelling evidence for the use of VL as the first choice in tracheal intubation and the use of apneic oxygenation during intubation, especially in the neonatal population, in today’s PAAD, Bai et al.,1 found in an on-line survey of clinical practice in North America, Europe, Asia Pacific, and South Asia that pediatric anesthesiologists have been slow to adopt these recommendations.
Many barriers to increased VL usage in the OR exist, including cost, availability, concerns about DL skills, and perhaps some degree of hubris. This is especially true, when looking internationally due to the potential for decreased availability of VL, which Bai and colleagues did. Additionally, we still struggle to convince some of our anesthesia colleagues (and even sometimes, our ICU and emergency medicine colleagues) about the benefits of VL on the first attempt. The argument that trainees, especially pediatric anesthesia fellows, need to know and be comfortably with DL in all age groups is valid. Equipment can break, malfunction, and not be available. Apneic oxygenation also has barriers to incorporation including increased equipment required, increased setup time, potentially increased plastic waste, and concerns regarding mask seal. So, what is the balance? Are we doing enough? And what are most of us doing currently?
Bai et al.1 developed a 21-question on-line survey with the help of survey specialists at the University of Michigan, SPA, PeDI, and the Scientific Committee of the Association of Pediatric Anaesthetists of Great Britain and Ireland. The survey received 900 responses from 6954 requests (12.9%) - which while a source of sampling bias was consistent with many other survey-based studies. Most of the respondents practiced primarily pediatric anesthesia (>70% of respondents) and had >10 years of experience post-training (>58% of respondents).
So, what did they find? First, video laryngoscopy is widely available with 93% of respondents indicating VL was “most likely available” in the main OR. However, outside of the main OR this availability decreases with only 80.1% of respondents indicating that VL was “most likely available” in non-OR locations. This feels like an area for significant improvement, as non-OR locations represent a unique place of vulnerability when managing the pediatric airway due to decreased resources and help.
When looking at neonatal and infant intubation, only 29% of respondents would very likely choose VL as first choice for premature and newborn infants. As infants aged, this percentage decreased. Respondents with >10 years of experience were less likely to choose VL, than their less experienced colleagues (26.4% vs. 33.1%, p=0.05). Additionally, those with low perceived VL availability, were less likely to choose VL than those with high perceived VL availability (17.8 vs. 31.7, p=0.002). However, despite respondents not always reaching for VL as their own first choice, 40% of respondents thought that VL should be standard of care in neonates. Again, there was a difference based on years of experience with those in practice >10 years being less likely to support that VL should be standard of care (36.9% vs. 45.5%, p = 0.013).
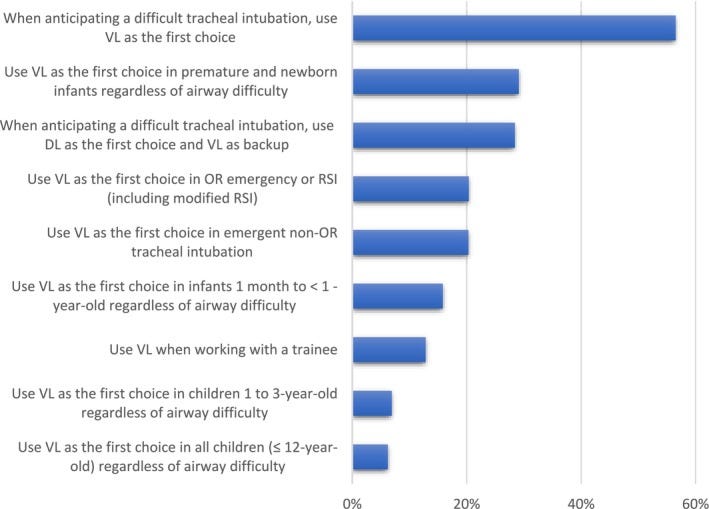
When faced with an anticipated difficult intubation in the OR, most respondents said they would most likely choose VL (56.5%), but perhaps surprisingly 30% of respondents said they would most likely first use DL and have VL as back-up. When intubating in emergency situations outside of the OR, only 33% of respondents said they would choose VL as their first choice.
Results were similar regarding apneic oxygenation usage. Here, respondents were asked if they would use apneic oxygenation during difficult tracheal intubation with only 30% agreeing that they would use this technique. Interestingly, 28.1% of respondents said they never use this technique.
With the presumed continued increasing availability of VL, where will our field settle? What is the right balance between training and patient outcomes? How do we maintain and teach critical skills while delivering the best outcomes to patients? Is there a risk that with full adoption of VL, we become too dependent on technology? Of course, we would be remiss to not remind readers that DL skills and teaching can still occur with VL when using traditional blades - perhaps this is the most ideal solution for the future.
Send your thoughts and comments to Myron who will post in a Friday reader response.
PS from Myron: As discussed in a previous PAAD (May 03, 2023 Videolaryngoscopy v Standard Direct Laryngoscopy https://ronlitman.substack.com/p/videolaryngoscopy-v-standard-direct ) that I will repost tomorrow, not all video laryngoscopes are created equal. there are differences in the make / model / size / angle/ “thickness” / “stickiness” - the list goes on - of VL blades plus differences in clinicians’ experience with these blades. The take home message: one VL blade is not the same as another VL blade – and knowing our airway equipment and our own skills and experience expertly enough to recognize these equipment limitations is critical to our success. Laryngoscopes – whether used for traditional DL or video systems can all fail.
References
1. Bai W, Koppera P, Yuan Y, Mentz G, Pearce B, Therrian M, Reynolds P, Brown SES: Availability and Practice Patterns of Videolaryngoscopy and Adaptation of Apneic Oxygenation in Pediatric Anesthesia: A Cross-Sectional Survey of Pediatric Anesthesiologists. Paediatr Anaesth 2025; 35: 460–468
2. Geraghty LE, Dunne EA, CM NC, Vellinga A, Adams NC, O'Currain EM, McCarthy LK, O'Donnell CPF: Video versus Direct Laryngoscopy for Urgent Intubation of Newborn Infants. N Engl J Med 2024; 390: 1885–1894
3. Muhs AL, Seitz KP, Qian ET, Imhoff B, Wang L, Prekker ME, Driver BE, Trent SA, Resnick-Ault D, Schauer SG, Ginde AA, Russell DW, Gandotra S, Page DB, Gaillard JP, Smith LM, Latimer AJ, Mitchell SH, Johnson NJ, Ghamande SA, White HD, Gibbs KW, Palakshappa JA, Vonderhaar DJ, Janz DR, Whitson MR, Barnes CR, Dagan A, Moskowitz A, Krishnamoorthy V, Herbert JT, April MD, Joffe AM, Walco JP, Hughes CG, Shipley K, Maiga AW, Lloyd BD, DeMasi SC, Self WH, Rice TW, Semler MW, Casey JD: Video vs Direct Laryngoscopy for Tracheal Intubation After Cardiac Arrest: A Secondary Analysis of the Direct vs Video Laryngoscope Trial. Chest 2025; 167: 1408–1415
4. Disma N, Asai T, Cools E, Cronin A, Engelhardt T, Fiadjoe J, Fuchs A, Garcia-Marcinkiewicz A, Habre W, Heath C, Johansen M, Kaufmann J, Kleine-Brueggeney M, Kovatsis PG, Kranke P, Lusardi AC, Matava C, Peyton J, Riva T, Romero CS, von Ungern-Sternberg B, Veyckemans F, Afshari A: Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Eur J Anaesthesiol 2024; 41: 3–23
5. Vukovic AA, Hanson HR, Murphy SL, Mercurio D, Sheedy CA, Arnold DH: Apneic oxygenation reduces hypoxemia during endotracheal intubation in the pediatric emergency department. Am J Emerg Med 2019; 37: 27–32
6. Riva T, Engelhardt T, Basciani R, Bonfiglio R, Cools E, Fuchs A, Garcia-Marcinkiewicz AG, Greif R, Habre W, Huber M, Petre MA, von Ungern-Sternberg BS, Sommerfield D, Theiler L, Disma N: Direct versus video laryngoscopy with standard blades for neonatal and infant tracheal intubation with supplemental oxygen: a multicentre, non-inferiority, randomised controlled trial. Lancet Child Adolesc Health 2023; 7: 101–111