It’s hard to believe, but January and February have come and gone and we are less than a month away from the Society for Pediatric Anesthesia-American Academy of Pediatric’s annual meeting to be held in Austin Texas March 31-April 2. If you haven’t already registered for the meeting please do it now!
https://www2.pedsanesthesia.org/forms/registration/2023winter_register.iphtml
For me, one of the highlights of the spring meeting occurs on the Friday of the meeting when the Robert M. Smith award is given to an individual who has made outstanding contributions to the field of pediatric anesthesiology. The award is named for Dr. Smith, often considered, the “father of pediatric anesthesia”, was one of the earliest American pioneers in pediatric anesthesiology, wrote and edited one of the first textbooks of pediatric anesthesia and was anesthesiologist-in-chief at the Boston Children’s Hospital from 1946-1980.
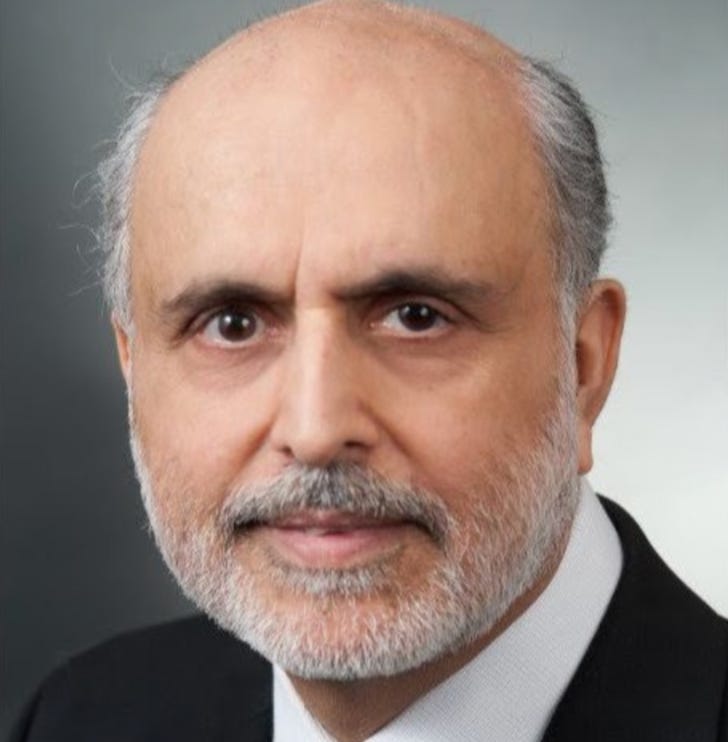
I am so happy, really thrilled, that this year’s Smith award winner is Navil Sethna MBchB of the Boston Children’s Hospital. Dr. Sethna is the Clinical Director, Pediatric Pain Rehabilitation Center; Senior Associate in Pain Medicine and Perioperative Anesthesia, Department of Anesthesiology, Critical Care and Pain Medicine and Professor of Anaesthesia, Harvard Medical School. Navil is without question one of the most outstanding clinicians, researchers, and teachers of his generation. I am simply over the moon that he is this year’s recipient of the Smith award and I am so lucky to be able to count him as one of my friends. I asked Dr. Gary Walco, Director, Pain Medicine and Professor of Anesthesiology and Pain Medicine at Seattle Children’s Hospital, University of Washington to pick an article that exemplifies Navil’s contribution to the field of pain medicine.
For those of you who know Navil, worked with him, or were one of his students or colleagues, please make every effort to attend and celebrate this award with him.
Myron Yaster MD
Original article
Navil F Sethna 1, Petra M Meier, David Zurakowski, Charles B Berde. Cutaneous sensory abnormalities in children and adolescents with complex regional pain syndromes. Pain. 2007 Sep;131(1-2):153-61. PMID: 17329025
I wish to congratulate my longtime colleague and friend, Navil Sethna, as the American Academy of Pediatrics Section on Anesthesiology and Pain Medicine recognizes him with the 2023 Robert M. Smith Award. My task was to review his bibliography and zero in on a single paper that I perceive made significant impact. That was no small task, as such a review highlighted Dr. Sethna’s versatility and his true spirit of collaboration, as he has partnered with an array of basic and clinical scientists covering a range of topics. After reflection, however, I recalled one paper that had a significant impact on me at the time it appeared, and it continues to serve a reminder of Dr. Sethna’s facility in building bridges to gain greater insight.
In 2007, Dr. Sethna was the principal author on a paper examining sensory abnormalities in children and adolescents with complex regional pain syndrome (CRPS). To put it in context, it was not so long before this that the syndrome was renamed from reflex sympathetic dystrophy (RSD) to CRPS and the International Association for the Study of Pain (IASP) published diagnostic criteria for adults. While many of us were recognizing this clinical entity in our pediatric pain programs, we had little insight into the degree to which the findings that drove that work were applicable to children and adolescents. Evidence seemed to indicate that were some notable differences between childhood and adults CRPS, such as affected limbs (lower limbs were more commonly affected in children, upper limbs for adults), female to male ratios, and, very importantly, a more positive prognosis in young patients, especially those treated in programs that combined physiotherapy and cognitive-behavioral paradigms targeting rehabilitation.
To better understand the nature of sensory abnormalities in children with this condition, Sethna and colleagues added quantitative sensory testing to the usual mix of medical history and physical examination data, thereby potentially giving greater insights into possible pathophysiology. While patterns of abnormal sensory perceptions paralleled those observed in adults, heat and cold allodynia were less frequent in the young. Further, there was a good deal of variability in detection thresholds of cold, warm, and vibration sensations, which overall were similar to control normal values. Sethna et al. tied this back to possible small fiber neuropathies, which had been discussed little in pediatrics up to that point. Very importantly, findings indicated a significant role of central sensitization in allodynia, more than peripheral changes per se.
So why was this paper so impactful? First, it showed the utility of QST in a clinical sample rather than healthy participants to better understand pathological processes. Few studies in children had done so prior. Second, it reinforced the notion that clinical syndromes that present in adults have elements in common with the presentation in children, but also some notable differences. This has implications for the diagnostic process, and various treatment decisions, especially when the limitations of extrapolation of adult treatment studies are under consideration. Third, it showed very clearly that focusing on only peripheral or only central mechanisms without looking at their interplay is short-sighted.
Interestingly, authors who have cited this work have had interests well beyond CRPS, including pain in juvenile arthritis, sickle cell disease, low back pain, and human and animal models of neuropathic pain. As the original authors indicated, by no means was this work definitive, but by all means it presented us with innovation in paradigms and strategies to better understand a complicated pain syndrome.
Congratulations Navil!
Gary A. Walco, PhD, Professor, Anesthesiology and Pain Medicine, Adjunct Professor Pediatrics; Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Director of Pain Medicine, Seattle Children's Hospital