Isolated Coarctation: Much Still To Be Learned
Susan Nicolson, Viviane Nasr, Lindsey Loveland, James DiNardo
Original article
Stephens EH, Feins EN, Karamlou T, Anderson BR, Alsoufi B, Bleiweis MS, d'Udekem Y, Nelson JS, Ashfaq A, Marino BS, St Louis JD, Najm HK, Turek JW, Ahmad D, Dearani JA, Jacobs JP. The Society of Thoracic Surgeons Clinical Practice Guidelines on the Management of Neonates and Infants With Coarctation. Ann Thorac Surg. 2024 Sep;118(3):527-544. doi: 10.1016/j.athoracsur.2024.04.012. Epub 2024 Jun 20. PMID: 38904587.
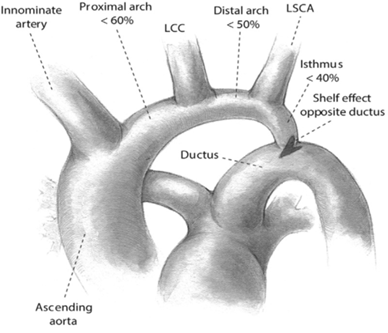
Coarctation of the aorta accounts for 4%-6% of patients with congenital heart disease and is the 2nd most common lesion requiring neonatal intervention. Despite being commonly encountered there is no consensus regarding the optimum management of isolated coarctation in neonates and infants. Isolated coarctation is defined as aortic coarctation that may have associated arch hypoplasia but without other congenital heart defects. Arch hypoplasia is said to be present when the z-score of the diameter of the distal transverse arch, the portion of the aorta between the left common carotid and left subclavian artery, <-2.0 (Figure 1). The heterogeneity in phenotype of isolated coarctation has been increasingly recognized, including variable severity of associated arch hypoplasia and arch anomalies. The STS Congenital Heart Surgery Task Force on Evidence Based Surgery assembled an expert multi-disciplinary panel (congenital cardiac surgeons, cardiologists and intensivists, no anesthesiologist) to formulate practice guidelines for isolated coarctation.
Figure 1. The most common aortic arch branching pattern found in humans with separate origins for innominate, left common carotid, and left subclavian arteries.
Key questions related to the care of these infants were identified using the PICO (Patients/Population, Intervention, Comparison/Control, Outcome) Framework. A PubMed search was performed, limited to studies published in English after 2000. Clinical practice guidelines were developed with classification of recommendation and level of evidence using a modified Delphi method (Table II). For a statement to reach consensus 80% of the members needed to vote with 75% of members who voted to agree.
Table II. Categories for Strength of Recommendation and Quality of Evidence1
Proposed Guidelines
1. Surgical repair recommended provided no surgical contraindications (COR: I, LOE: B-MR)
a. Via thoracotomy when isolated coarctation without arch hypoplasia (COR: I, LOE: C-EO)
b. Via sternotomy with arch hypoplasia that cannot be addressed via thoracotomy (COR: IIa, LOE: B-NR)
c. Via sternotomy with variant of aortic arch branching where the left common carotid artery originates separately from the innominate artery (Figure 2) (COR: IIb, LOE: C-LD)
d. With sternotomy
· antegrade cerebral perfusion or limited-duration deep hypothermic circulatory arrest (COR : IIb, LOE:B-R)
· end-to-end, arch advancement, and patch augmentation – all reasonable techniques (COR: IIa, LOE: B-NR)
2. Medical optimization is recommended before primary operation or intervention when risk factors (prematurity, low birth weight, decreased LV function, intraventricular hemorrhage) are present (COE: IIa, LOE: B-NR)
Figure 2. Variant of aortic arch branching where left common carotid originates separately from the innominate. Many erroneously refer to this as a “bovine arch”
Figure 3 depicts the branching pattern seen in medium to large ungulates: reindeer, cattle bison, buffalo, and antelope, a true “bovine arch”, which differs significantly from what many clinicians call a “bovine arch” in humans (Figure 2).2
Figure 3. Branching pattern found in cattle has a single brachiocephalic trunk and splits into bilateral subclavian arteries and a bi-carotid trunk.
There are limitations of the data the panel had to review including: lack of randomized trials, small sample sizes, inconsistent definition of diagnoses, procedures and outcomes, and implicit selection bias within single institution case series as regards technique. Thus, recommendations need to be taken in the context of the individual neonate or infant as well as the expertise of a given surgeon and the program where they work.
Research is needed to correlate the type of operation with the eventual shape of the arch, to assess the effect of patch material and other modifiable surgical factors on distensibility of the arch and flow patterns and to associate these with late morbidity. The focus needs to include long-term outcomes including the incidence of hypertension, health-related quality of life and neurodevelopment outcomes while continuing to determine short-term outcomes and perioperative complications.3 Significant opportunities remain to better delineate optimal management of these patients.
Send your thoughts and comments to Myron who will post in a Friday Reader Response
References:
1. Isselbacher EM, Preventza O, Hamilton Black J, 3rd, et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2022;146(24):e334-e482. (In eng). DOI: 10.1161/cir.0000000000001106.
2. Layton KF, Kallmes DF, Cloft HJ, Lindell EP, Cox VS. Bovine aortic arch variant in humans: clarification of a common misnomer. AJNR American journal of neuroradiology 2006;27(7):1541-2. (In eng).
3. Chiu P, Gearhart A, Gikandi A, et al. Sternotomy or thoracotomy for neonatal repair of coarctation of the aorta with aortic arch hypoplasia. JTCVS Open 2024;22:386-394. DOI: https://doi.org/10.1016/j.xjon.2024.10.001.