Over the past couple of months, the PAAD has reviewed several articles from the Journal Pediatric Anesthesia on “error traps in anesthesia practice”. I realized that a PAAD dedicated to explaining what error traps are was long overdue. So, I asked Dabe Chatterjee who was the journal of Pediatric Anesthesia’s editor for this series of articles to go back to the original articles by Stiegler et al.1, 2 to review them for the PAAD community. Together with his colleague Dr. Gina Whitney they’ve provided this concise explanation and review. Myron Yaster MD
Original articles
Stiegler MP, Neelankavil JP, Canales C, Dhillon A. Cognitive errors detected in anaesthesiology: a literature review and pilot study. Br J Anaesth. 2012 Feb;108(2):229-35. PMID: 22157846
Stiegler MP, Tung A. Cognitive processes in anesthesiology decision making. Anesthesiology. 2014 Jan;120(1):204-17. PMID: 24212195
The study of how we make decisions, particularly under stressful situations, has received much attention in the safety literature. Within the last ten years, the study of how we make clinical decisions as anesthesiologists has begun to receive increasing attention. If you have a long flight coming up, Gary Klein’s book, Sources of Power, is an excellent overview of the science of decision-making, particularly during emergencies. Much of the work focuses on the study of firefighters, and you’ll quickly see the parallels in crisis management and the influence of experience – it’s a fascinating read.
Cognitive errors are “thought-process errors, usually linked to failed biases or heuristics.”1 Biases are “systematic preferences to exclude certain perspectives on decision possibilities.”2 They result from subconscious influences from life experiences and individual preferences. Heuristics are “cognitive shortcuts used by humans to reduce the cognitive costs of decision making. “2 While both heuristics and biases are frequently used in medicine to make quick clinical decisions, cognitive errors occur when these subconscious processes and mental shortcuts are relied upon excessively or used under the wrong circumstances.1 It is important to note that cognitive errors are not knowledge gaps.
Cognitive errors have been described in many other specialties and are thought to contribute to patient harm and misdiagnoses far more than technical errors. In fact, more than two-thirds of missed or delayed diagnoses are caused by cognitive errors. Over 100 different types of cognitive errors have been described, many of which may contribute to adverse patient outcomes. A study by Stiegler et al. published in the British Journal of Anaesthesia in 2012 was the earliest effort to understand how cognitive errors may impact decision-making within the practice of anesthesiology.1
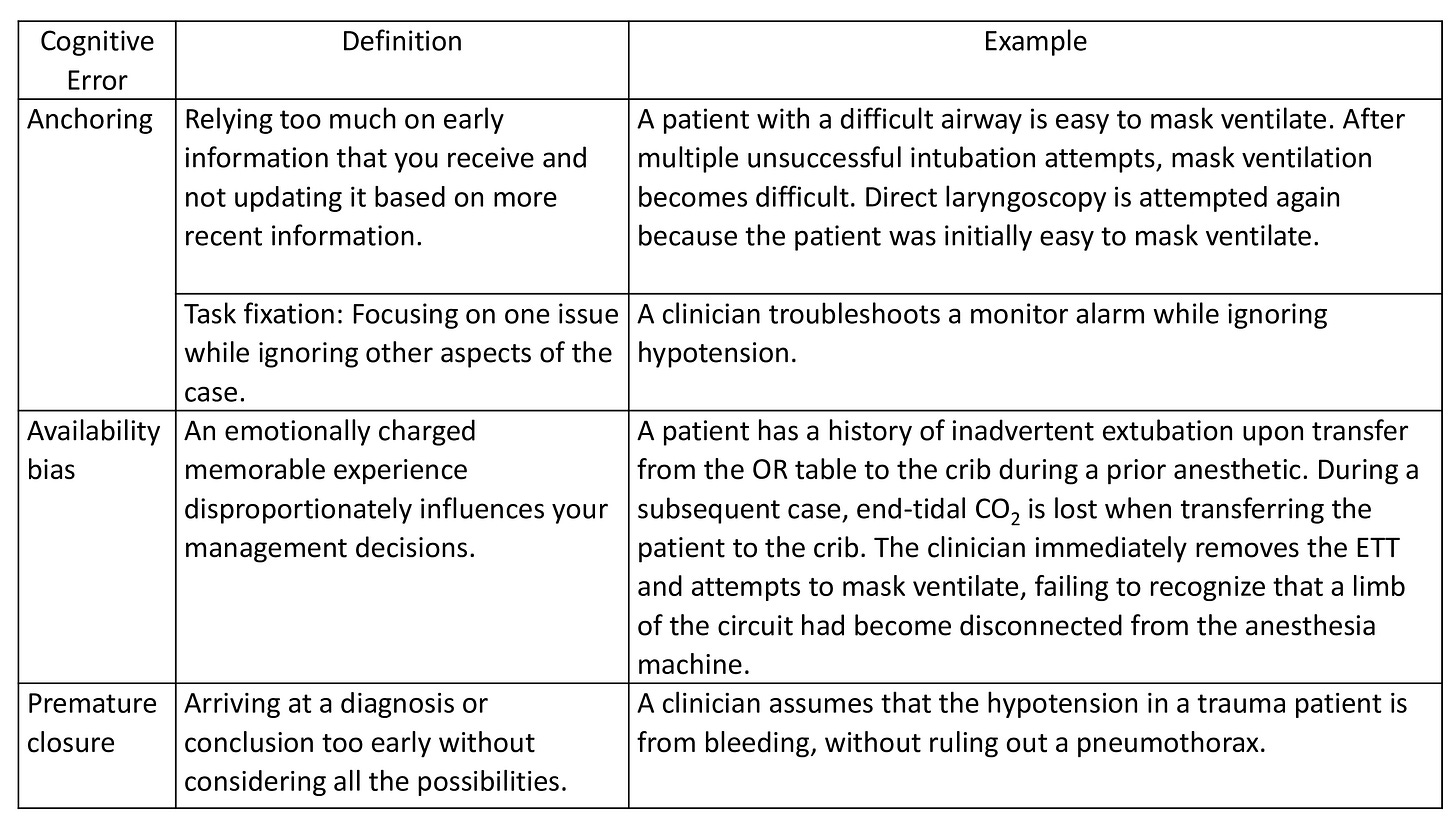
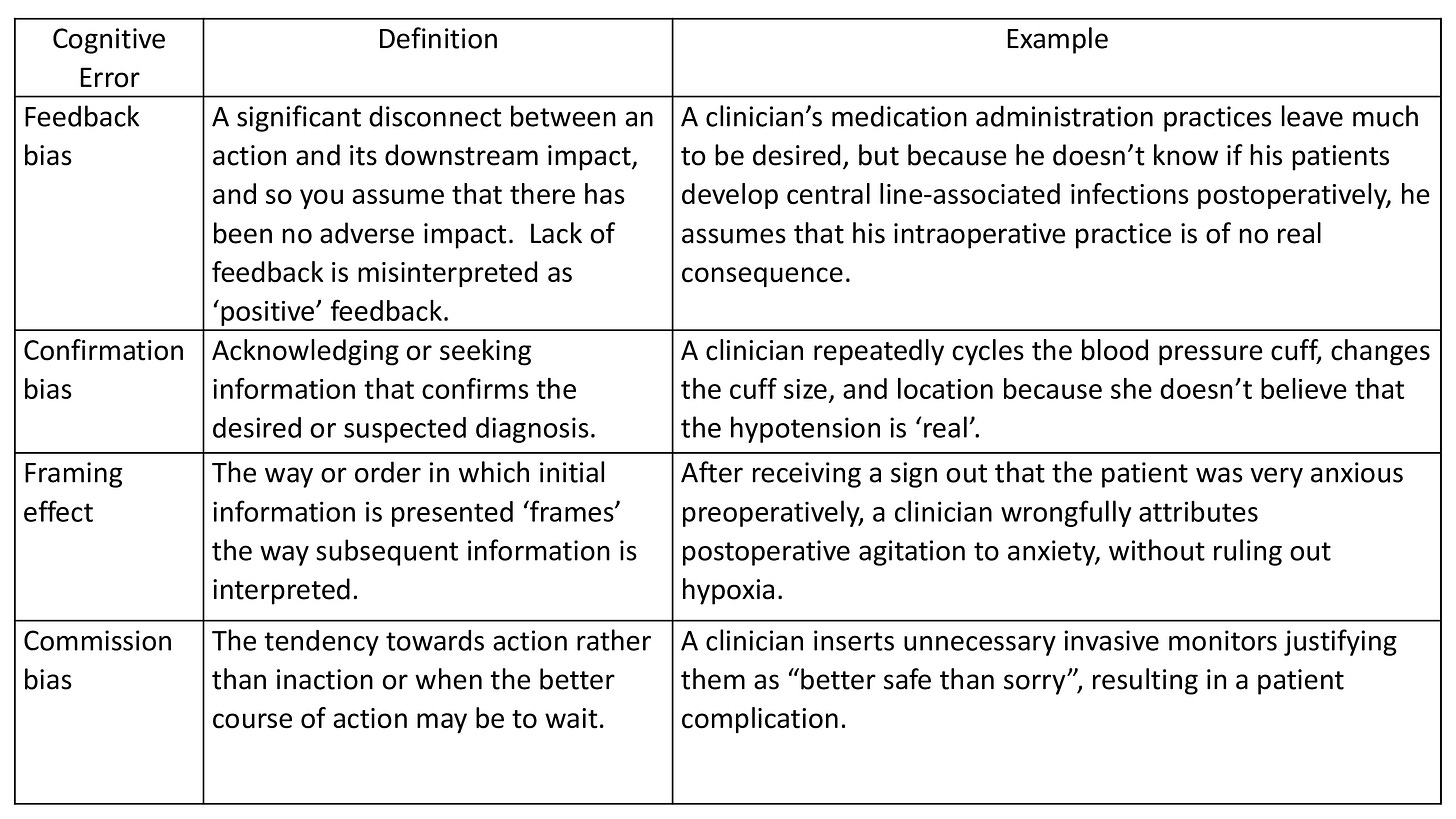
The authors first created a catalog of anesthesiology-specific cognitive errors and then used the modified Delphi method and faculty surveys to narrow it down to 10 cognitive errors within the practice of clinical anesthesiology (Tables 1-3).1 In the second part of the study, the authors observed 32 resident physicians managing simulated anesthesiology emergencies to identify these cognitive errors. Seven of the nine types of cognitive errors (premature closure, confirmation bias, sunk costs, commission bias, omission bias, anchoring, and overconfidence) were observed in over half of the simulation sessions. The contribution of cognitive errors to imperfect decision-making was made clear in both interviews with faculty and observation of simulated emergency scenarios.
So, how can we reduce these cognitive errors? The dual process theory of clinical decision making and strategies to reduce cognitive errors will be discussed in a future PAAD.
References:
1. Steigler MP, Neelankavil JP, Canales C, et al. Cognitive errors detected in anaesthesiology: a literature review and pilot study. British Journal of Anaesthesia. 2012;108(2): 229-35.
2. Steigler MP, Tung A. Cognitive processes in anesthesiology decision making. Anesthesiology. 2014; 120:204-17.
3. Webster CS, Taylor S, Weller JM. Cognitive biases in diagnosis and decision-making during anaesthesia and intensive care. BJA Education. 2021;21(11): 420-25.