I hope you’ve all had wonderful Thanksgiving celebrations with your families and for our Jewish readers lots of latkes and candle lighting during this Chanukah week! The PAAD is back and we will continue to publish on our regular schedule till Christmas and New Year’s week.
As anesthesiologists we diagnosis and treat anemia on a daily basis. What is the “trigger” hemoglobin/hematocrit that requires our intervention? And why? In pediatrics do we even know? The strong association of anemia and perioperative morbidity and mortality has traditionally guided our thinking on this topic.(1,2) I know this is going to be hard form many of you ‘youngins’ to believe, but when I started out, surgery and anesthesia were routinely cancelled or delayed for hemoglobins less than 10. Could you imagine doing that today? Red blood cell transfusions were given much more liberally until the infectious risks of transfusions, in reality AIDS and Hepatitis, made us rethink our practices. Then the risks of transfusion induced lung injury further made us even more gun shy. Times have clearly changed but how low can you go before you need to intervene? In the November 16th PAAD, “Association is not Causation” our pediatric anesthesia cardiac reviewers (including Lindsey Loveland Baptist, the primary reviewer of today’s PAAD) discussed the article by Justin Long et al. “Postoperative Hematocrit and Adverse Outcomes in Pediatric Cardiac Surgery Patients: A Cross-Sectional Study From the Society of Thoracic Surgeons and Congenital Cardiac Anesthesia Society Database Collaboration. Anesth Analg. 2021 Nov 1;133(5):1077-1088. PMID: 33721876) and its associated editorial. Over the next 2 days we will review some of these issues in the non-cardiac population in much greater detail. Myron Yaster MD
Original article
Gregory M. T. Hare, C. David Mazer; Anemia: Perioperative Risk and Treatment Opportunity. Anesthesiology 2021; 135:520–530 PMID: 34197591
Today’s PAAD is a clinical focus review from the journal Anesthesiology. Although this article is focused entirely on adult patients we think it is so important that we’ve made it today’s PAAD. This article outlines the many perioperative systemic effects that occur in the 30% (yes 30%!) of adult patients who present for surgery chronically anemic (men <13g/dl, and women <12g/dl),(3) or who develop acute intraoperative anemia (blood loss and hemodilution from overly aggressive fluid resuscitation), and postoperative anemia. The harmful effects of anemia are highlighted across multiple organ systems, which parallel the negative effects of over transfusion highlighted in the recent PAAD article. We highly recommend reading the entire review article and if you are in a teaching program distributing this (and tomorrow’s article and our PAAD comments) to your students.
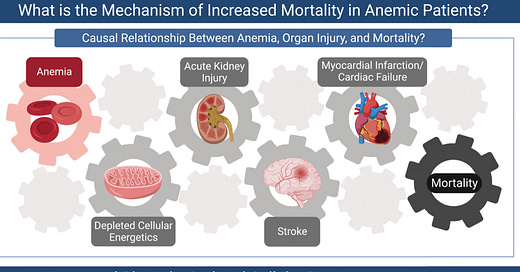
“Understanding the mechanism(s) of organ injury and death associated with anemia is central to developing, and applying, effective treatments in an attempt to prevent adverse outcomes”.(4) Some quick basic physiology review points: O2 delivery to the tissues is the product of cardiac output (CO) and O2 content (CaO2). CaO2 is primarily related to hemoglobin/hematocrit and O2 saturation (the amount of dissolved O2 in the blood except in rare circumstances is pretty negligible). Organ injury/ischemia occurs when O2 delivery and consumption (VO2) are out of balance. When O2 delivery fails to meet VO2 demands, physiologic adaptations to increase delivery, such as increased cardiac output, redistribution of cardiac output to vulnerable organs, or increased O2 extraction occur immediately. Some organs, like the brain and heart, maximally extract O2 at rest so increasing extraction in those critical organs is limited making them most vulnerable to the effects of anemia. At the cellular level, production of hypoxia inducible factor (HIF) occurs in all cells to contribute to cellular adaptation (see more about HIF below).
The association between anemia and adverse outcomes have been reported in large retrospective studies -again presenting us the challenge of teasing apart causation vs association.(1,2) A retrospective analysis of ~230,000 patients from the National Surgical Quality Improvement Program database demonstrated a nearly 30% rate of chronic anemia (~70,000 patients).(5) These anemic patients had an increased odds ratio for mortality, cardiac injury, respiratory dysfunction, and renal injury.(5) A similar international database again demonstrated ~30% rate of patients had anemia preoperatively, and an increased risk of in hospital mortality and myocardial infarction. A third analysis of 19,000 patients demonstrated a 31% rate of anemia and increased risk of mortality.(1) Amongst patients undergoing cardiac surgery, anemia was independently associated with an increased risk of stroke, death, and acute kidney injury.(6) In summary, if the severity of anemia is stratified; the greater the magnitude of anemia, the greater the risk of in-hospital death, stroke, and acute kidney and myocardial injury.
Because pre and intra operative anemia are the strongest predictors of intraoperative transfusion, it is difficult to separate risk of anemia from that of transfusion.(6) Both are associated with adverse outcomes. An important element of this review involved HIF, “the master genetic regulator of hypoxic cellular responses”.(7) It is beyond the scope of today’s PAAD to discuss the role of the peripheral O2 chemoreceptors in the carotid bodies and the role of HIF in O2 homeostasis, but if you like we can review this in more detail in a future PAAD. Just let us know.
There have been multiple recent studies looking at transfusion triggers in the OR with trials looking at restrictive versus liberal approaches to erythrocyte transfusion.(8) Clearly different populations and procedures and the speed of blood loss and potential for more blood loss generate different transfusion strategies. In pediatrics there is really very little data from RCTs to guide us. We do know that when hemoglobin levels fall below 5, organ system failure occurs. In our practice we use 7 as our trigger IF blood loss is controlled and not ongoing. In active bleeding is occurring we transfuse at higher hemoglobin concentrations but more on this in tomorrow’s PAAD.
The attached figure from the article is terrific and summarizes the physiologic responses to anemia.
References
1. Fowler AJ, Ahmad T, Abbott TEF, Torrance HD, Wouters PF, De Hert S, Lobo SM, Rasmussen LS, Della Rocca G, Beattie WS, Wijeysundera DN, Pearse RM. Association of preoperative anaemia with postoperative morbidity and mortality: an observational cohort study in low-, middle-, and high-income countries. Br J Anaesth 2018;121:1227-35.
2. Turan A, Cohen B, Rivas E, Liu L, Pu X, Maheshwari K, Farag E, Onal O, Wang J, Ruetzler K, Devereaux PJ, Sessler DI. Association between postoperative haemoglobin and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Br J Anaesth 2021;126:94-101.
3. Warner MA, Shore-Lesserson L, Shander A, Patel SY, Perelman SI, Guinn NR. Perioperative Anemia: Prevention, Diagnosis, and Management Throughout the Spectrum of Perioperative Care. Anesth Analg 2020;130:1364-80.
4. Hare GMT, Mazer CD. Anemia: Perioperative Risk and Treatment Opportunity. Anesthesiology 2021;135:520-30.
5. Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A, Khreiss M, Dahdaleh FS, Khavandi K, Sfeir PM, Soweid A, Hoballah JJ, Taher AT, Jamali FR. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet 2011;378:1396-407.
6. Klein AA, Collier TJ, Brar MS, Evans C, Hallward G, Fletcher SN, Richards T. The incidence and importance of anaemia in patients undergoing cardiac surgery in the UK - the first Association of Cardiothoracic Anaesthetists national audit. Anaesthesia 2016;71:627-35.
7. Prabhakar NR, Semenza GL. Oxygen Sensing and Homeostasis. Physiology (Bethesda) 2015;30:340-8.
8. Hare GMT, Cazorla-Bak MP, Ku SFM, Chin K, Mistry N, Sklar MC, Pavenski K, Alli A, Van Rensburg A, Friedrich JO, Baker AJ, Mazer CD. When to transfuse your acute care patient? A narrative review of the risk of anemia and red blood cell transfusion based on clinical trial outcomes. Can J Anaesth 2020;67:1576-94.