Airway management in neonates and infants – ESAIC and BJA joint guidelines: Part 2
Mary Lyn Stein, MD, FAAP and James M. Peyton MBChB, MRCP, FRCA
Nothing is more fundamental in our role as pediatric anesthesiologists as our expertise in airway management in general, and in neonates and infants, in particular. Dr. Francis Veyckemans alerted me to this article1,2 which is written by a who’s who of pediatric airway experts and was published jointly by the European J Anaesthesiology and the British J of Anaesthesiology. I asked Drs. Mary Lyn Stein and Jamie Peyton of the Boston Children's Hospital to review it for us. Jamie is a frequent contributor to the PAAD and was one of the authors of the paper. Finally, because of its length and my desire to keep PAADs to 5 to 6 minute reads, I’ve split the discussion into 2 parts. I posted part one yesterday, here is part 2. Myron Yaster MD
Original article
Disma N, Asai T, Cools E, Cronin A, Engelhardt T, Fiadjoe J, Fuchs A, Garcia-Marcinkiewicz A, Habre W, Heath C, Johansen M, Kaufmann J, Kleine-Brueggeney M, Kovatsis PG, Kranke P, Lusardi AC, Matava C, Peyton J, Riva T, Romero CS, von Ungern-Sternberg B, Veyckemans F, Afshari A; and airway guidelines groups of the European Society of Anaesthesiology and Intensive Care (ESAIC) and the British Journal of Anaesthesia (BJA). Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Eur J Anaesthesiol. 2024 Jan 1;41(1):3-23. doi: 10.1097/EJA.0000000000001928. Epub 2023 Dec 13. PMID: 38018248; PMCID: PMC10720842.
Disma N, Asai T, Cools E, Cronin A, Engelhardt T, Fiadjoe J, Fuchs A, Garcia-Marcinkiewicz A, Habre W, Heath C, Johansen M, Kaufmann J, Kleine-Brueggeney M, Kovatsis PG, Kranke P, Lusardi AC, Matava C, Peyton J, Riva T, Romero CS, von Ungern-Sternberg B, Veyckemans F, Afshari A; airway guidelines groups of the European Society of Anaesthesiology and Intensive Care (ESAIC) and the British Journal of Anaesthesia (BJA). Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Br J Anaesth. 2024 Jan;132(1):124-144. doi: 10.1016/j.bja.2023.08.040. Epub 2023 Nov 29. PMID: 38065762.
5 – Apply apneic oxygenation during tracheal intubation in neonates (Strong recommendation, medium quality of evidence 1B)
Now this one gets at a different interesting issue – my guess is that there aren’t many readers who would argue that providing apneic oxygenation is a bad idea. The evidence seems quite clear that supplemental oxygen extends the time before the onset of hypoxemia, but many of us don’t routinely use it. Why? Some have argued that the presence of a nasal cannula interferes with mask seal. We’ve certainly seen people struggle with this, but have found that with a slight change in technique (switch to two handed thumb and forefinger mask for example) we can generally overcome the leak. Our own practice is to keep nasal cannula oxygen on anyone who already has it on and to add it for anyone we think is at risk for rapid onset of hypoxemia (e.g. pulmonary pathology, obesity, etc) and anyone we think will take longer than ~30 seconds to intubate (difficult airway, inexperienced laryngoscopist, etc). For the inexperienced laryngoscopist, we find that it prolongs the time until the drop in the pulse oximeter’s tone and ensuing catecholamine surge in the clinician!
6 – Consider a supraglottic airway for rescue oxygenation and ventilation when tracheal intubation fails (Strong recommendation, medium quality of evidence 1B)
We think this is a near universal recommendation at this point (https://ronlitman.substack.com/p/difficult-or-impossible-face-mask) and it’s not a question of “is this a good idea?” but “how do we remind ourselves to do it?” When I (MLS) was first starting out as an attending, I’d put an #1 LMA Unique out next to the laryngoscope for every single baby intubation. I felt like it lowered the activation energy to get it and use it. I used it a handful of times and was so grateful that I wasn’t going back to the cart looking for it in those moments. I also think it trained my stressed, flight or fight brain into a behavioral pattern or “muscle memory” - to put down the laryngoscope and pick up the LMA. Indeed, the PeDIR data shows that we do not use LMAs enough when intubation has initially failed. It seems to be a universal recommendation, but it is not something that is being used as much as it should be even in hospitals within the registry where you would expect a high degree of use.
7 – Limit the number of tracheal intubation attempts (Strong recommendation, low quality of evidence 1C)
We could write almost the exact same comment as for 6. We don’t think there’s any question that we want to limit the number of attempts for patient safety. The real question is what to do when we’re trying out best and it’s not working? The task force recommends stopping and emerging the patient after 4 attempts. As with everything we do, this is going to be patient and situation dependent, but I think it’s advisable to have a plan of when to stop and what the contingency plans are ahead of time – yes – even for routine airways! Make sure to change something (blade or device, positioning, laryngoscopist, etc) with each attempt and know what your stopping point will be.6.
8 – Use a stylet to reinforce and preshape the tracheal tubes when hyperangulated videolaryngoscope blades are used and when the larynx in anatomically anterior (Strong recommendation, low quality of evidence 1C)
This is a point about geometry not the relative merits of a stylet for a standard blade in an anatomically normal airway. Hyperangulated blades allow a video view around a corner – they are not designed to be used with straight or slightly curved endotracheal tubes and clinicians will struggle to get the tube to the view they can clearly see on the screen without an appropriately angled stylet.
9 – Verify intubation is successful with clinical assessment and end-tidal CO2 waveform (Strong recommendation, low quality of evidence 1C)
Continuous waveform capnography is a standard anesthetic monitor and in our opinion is mandatory for verification of successful intubation. It’s been discussed in prior PAADs (https://ronlitman.substack.com/p/capnography-for-all-a-call-to-action) and rather than repeating that discussion we’d like to ask readers to consider making a donation to LIFEBOX (www.lifebox.org) to ensure this critical monitor is more widely available.
10 – Apply high-flow nasal oxygenation, CPAP, or NIPPV for post extubation respiratory support, when appropriate (Strong recommendation, medium quality of evidence 1B)
This is another interesting one and something that our dual pediatric ICU/anesthesia colleagues recently reviewed (https://ronlitman.substack.com/p/what-is-the-most-effective-post-extubation). As we’ve already gone on for far too long, we’ll refer you to their excellent discussion.
Send your thoughts and comments to Myron who will post in a Friday Reader response.
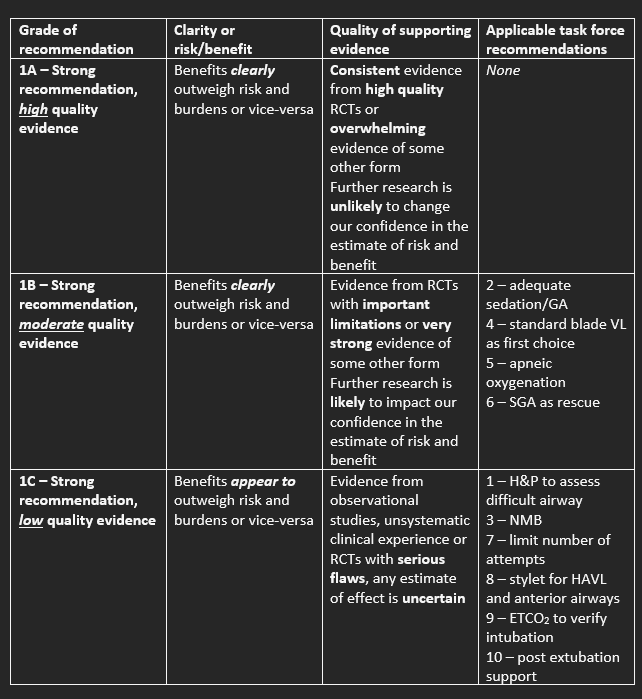
Table. Summary of Grade recommendations and applicable task force recommendations
References
1. Disma N, Asai T, Cools E, et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. British journal of anaesthesia 2024;132(1):124-144. (In eng). DOI: 10.1016/j.bja.2023.08.040.
2. Disma N, Asai T, Cools E, et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. European journal of anaesthesiology 2024;41(1):3-23. (In eng). DOI: 10.1097/eja.0000000000001928.
3. Habre W, Disma N, Virag K, et al. Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir Med 2017;5(5):412-425. DOI: 10.1016/S2213-2600(17)30116-9.
4. Disma N, Virag K, Riva T, et al. Difficult tracheal intubation in neonates and infants. NEonate and Children audiT of Anaesthesia pRactice IN Europe (NECTARINE): a prospective European multicentre observational study. British Journal of Anaesthesia 2021. DOI: 10.1016/j.bja.2021.02.021.
5. Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med 2016;4(1):37-48. (In eng). DOI: 10.1016/s2213-2600(15)00508-1.
6. Sohn L, Peyton J, von Ungern-Sternberg BS, Jagannathan N. Error traps in pediatric difficult airway management. Paediatric anaesthesia 2021;31(12):1271-1275. (In eng). DOI: 10.1111/pan.14289.