I guess because I grew up without any money, I am by nature someone who is “frugal” (not that you’d know it if you looked at my Amex statements). I’m sure my kids hated it when I would say: “Hey, do you think we’re Rockefellers? Turn off the expletive deleted lights when you leave a room!” I still do this and I’m sure it’s one of the many things that drives my wife Pam crazy. The hospital in general and the ORs and the PICU in particular are the worst! How many time would I arrive to the OR in the morning to do my machine checkout and find the oxygen freely flowing from an anesthesia machine and from its safety side oxygen backup flow meter. And don’t get me started with the PICU at which every bed had oxygen flowing for the emergency bag mask system and ventilators running at 60 L/minute. Thus, today’s article by Kinthala et al.1 immediately caught my eye. Myron Yaster MD
Original article
Kinthala S, Yepuri N, Senapathi SH, Ali N, Madabhushi P. Oxygen wastage in operating room and clinical units after hours: A quality improvement project from a single tertiary care institution. J Clin Anesth. 2023 Sep;88:111118. doi: 10.1016/j.jclinane.2023.111118. Epub 2023 Apr 13. PMID: 37060731
As we’ve discussed in several previous PAADs, the operating rooms and the pre-post anesthesia care units are major sources of hospital waste. Just think about all of the single use disposables and their associated plastic wrapping. Kinthala et al. wondered if an educational program would reduce wasted oxygen from flow meters and anesthesia machines that were not turned off at the end of the work day.
Using an educational quality improvement project, they looked at oxygen wastage before and after their intervention. The educational intervention detailed the background of the study and the specific need for attention in turning off oxygen flowmeters when not in use and included 80 anesthesiologists, nurse anesthetists, perioperative nurses, and anesthesia technicians in a single institution. The total oxygen wastage was calculated and converted to dollars by multiplying wastage with procurement cost of oxygen at their organization.
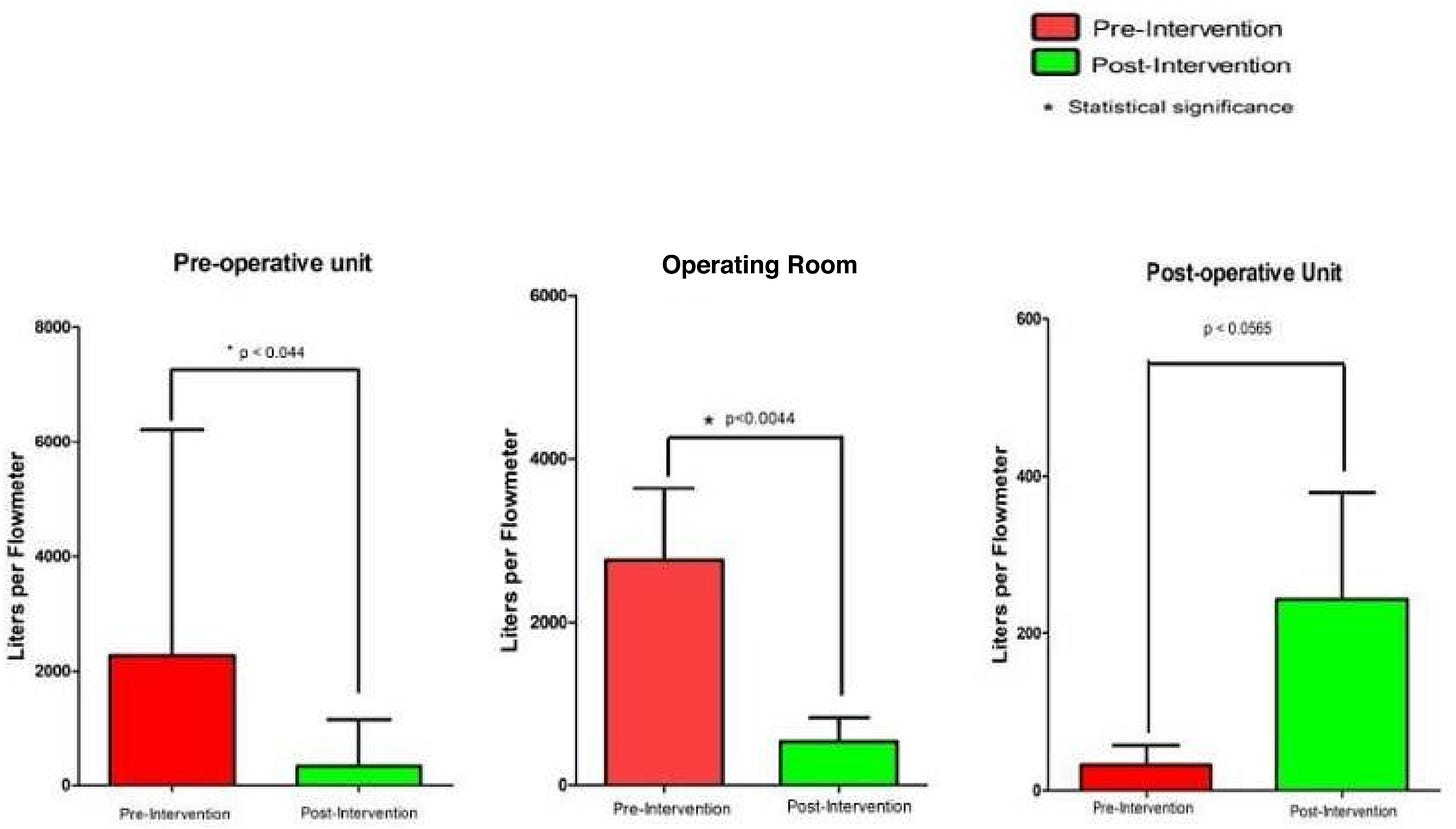
As can be seen in the figure, oxygen wastage was significantly reduced in the preop unit and the ORs but actually increased in the postop units. Why it increased in the post op areas is unclear, but the authors attributed it to personnel turnover in those units during the period after the intervention. The amount of money saved by reducing the oxygen waste was substantial. Whether the authors were able to maintain their results after the study period is unknown as surveillance was discontinued after the post-intervention assessment. This is a serious omission. Positive change will occur when the troops know they are being watched (the Hawthorne effect). Will it be sustained when no one is looking? This is one of the lessons that Dr. Lynn Martin and his implementation science colleagues in Seattle have taught us over the past couple of years.
We think this is a terrific opportunity for members of SPA, SPA’s sustainability SIG, and project SPRUCE Forest. As we hope you recall, Project SPRUCE Forest uses implementation science methods to achieve or surpass their goal of 50% reduction in green house gas emissions in each participating center over 12 months. The principal investigators are Drs. Elizabeth Hansen and Diane Gordon.
What do you think? Can you attempt to replicate these results at your own institution or do you have a similar project already underway? Let Myron know and he will post in Friday’s Reader Response.
References
1. Kinthala S, Yepuri N, Senapathi SH, Ali N, Madabhushi P. Oxygen wastage in operating room and clinical units after hours: A quality improvement project from a single tertiary care institution. Journal of clinical anesthesia. 2023/09/01/ 2023;88:111118. doi:https://doi.org/10.1016/j.jclinane.2023.111118