A better LMA in our future?
Myron Yaster MD and Melissa Brooks Peterson MD
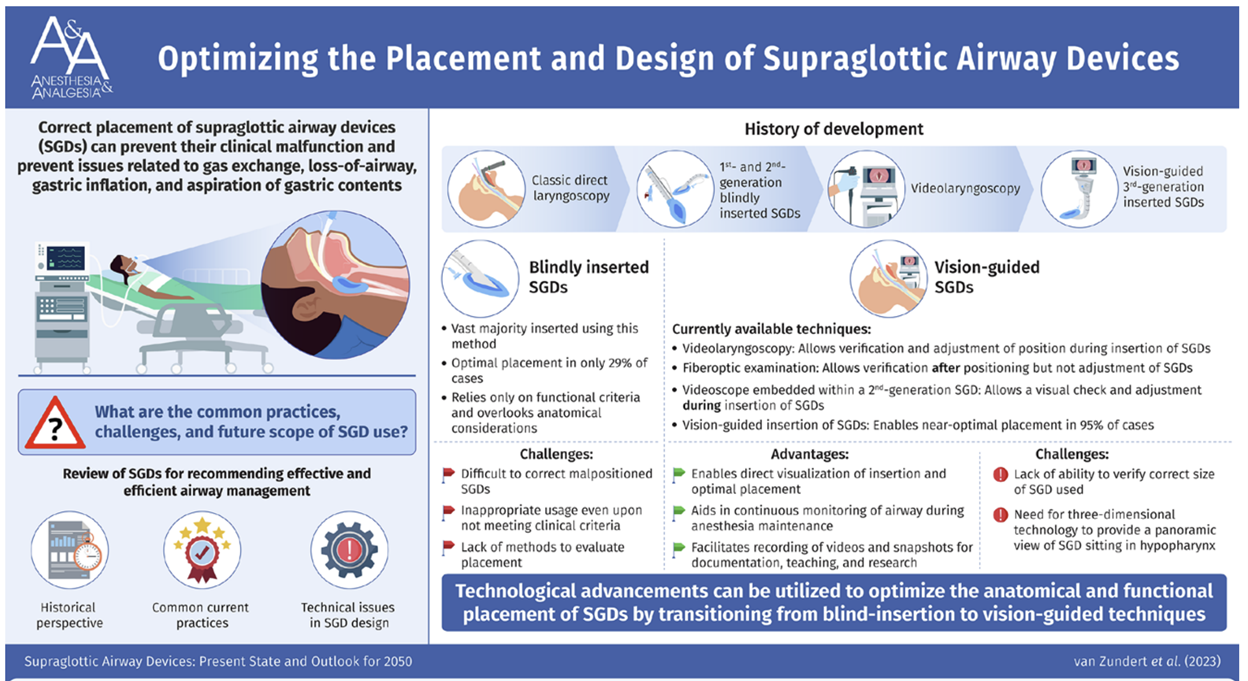
Long before the introduction of the LMA, managing the airway came down to either tracheal intubation or using a face mask. Indeed, early on in my residency in anesthesiology while discussing my anesthetic plan with my attending, I said that I would like to intubate the trachea because the procedure was going to last more than 2 hours. He replied by pointing out that “that the length of a case [was] not an indication for intubation” and he made me do the case by mask to prove a point (or maybe he was simply a sadist). Although my hand was in spasm at the conclusion of the case, I really did learn important lessons on how to hold a mask properly and maintain a tight seal. Fortunately, Dr. Archie Brain 1 in the 1980s revolutionized airway management with the brilliant and groundbreaking concept of the laryngeal mask airway (LMA). With the advent of the LMA, we had a way to create a seal over the laryngeal inlet and anesthesia has never been the same. In today’s PAAD, van Zundert et al.2 reviews much of the history behind supra glottic airways (SGAs) and imagines a radical and improved redesign. I thought it was interesting enough for the PAAD particularly because the accompanying figure below is outstanding and may be of use to many of you who teach or lecture on this topic to various audiences. Myron Yaster MD
Original article
van Zundert AAJ, Gatt SP, van Zundert TCRV, Hagberg CA, Pandit JJ. Supraglottic Airway Devices: Present State and Outlook for 2050. Anesth Analg. 2024 Feb 1;138(2):337-349. doi: 10.1213/ANE.0000000000006673. Epub 2024 Jan 12. PMID: 38215712.
Today’s PAAD by Van Zundert et al.2 opens by stating that “this article emphasizes that the correct placement of supraglottic airway devices (SGDs) is as important as the proper positioning of endotracheal tubes (ETTs) and that optimal SGD placement and positioning is best facilitated by direct vision.” As you all know, SGAs are placed blindly and malpositions are more common than we’d like to admit and are not easily visualized.2,3 “Brimacombe described 7 well-recognized malpositions: (1) epiglottic downfolding; (2) infolding of aryepiglottic folds; (3) rotation in the sagittal plane with respect to the pharynx or larynx; (4) backward folding of the distal cuff; (5) glottis distortion; (6) distal; as well as (7) proximal cuff misplacement. Any or all these anatomical misplacements can still result in clinical signs suggesting proper positioning.”2,3
Would a better, novel design be better? Van Zundert et al suggest a new device video supraglottic device (SGD) “where the (fiberoptic) camera is at the appropriate tip of the SGD, and this permits, in theory, insertion under videoscopy of a deflated SGD, pressed against the hard palate, following the curve of the tongue and placed between tongue base and hypopharynx, followed by manipulation of the SGD into the pharynx, such that the SGD tube opening faces the glottic opening. Under continuous monitoring of the device, the cuff is inflated using a cuff pressure monitor (ideal range 40–60 cm H2O) and visual checking whether the SGD continues to sit correctly after cuff inflation. Clinical signs should all also be checked and for further anatomical confirmation, a fiberoptic scope can be used.”2 Further, when using a video SGD as a conduit for intubation, one would be able to visualize the insertion of the ETT into the trachea AND insure that the ETT is advanced to the correct depth!
All I (Myron) can say is “wow”, “what a clever idea”, and “we can’t wait to get our hands on one of these!” Mel’s immediate thoughts are “I’d really like to try this out for myself,” “this sounds very complicated [read: expensive] for a likely disposable device,” “I wonder what the NNT is for repositioning and cost/benefit analysis,” and “an inflation pressure of 40-60 sounds painful just reading it, let alone against a child’s pharynx”
What do you think? Send your thoughts to Myron who will post in a Friday reader response
References
1. Brain AI. The laryngeal mask--a new concept in airway management. British journal of anaesthesia 1983;55(8):801-5. (In eng). DOI: 10.1093/bja/55.8.801.
2. van Zundert AAJ, Gatt SP, van Zundert T, Hagberg CA, Pandit JJ. Supraglottic Airway Devices: Present State and Outlook for 2050. Anesthesia and analgesia 2024;138(2):337-349. (In eng). DOI: 10.1213/ane.0000000000006673.
3. Van Zundert AA, Kumar CM, Van Zundert TC. Malpositioning of supraglottic airway devices: preventive and corrective strategies. British journal of anaesthesia 2016;116(5):579-82. (In eng). DOI: 10.1093/bja/aew104.